Abstract
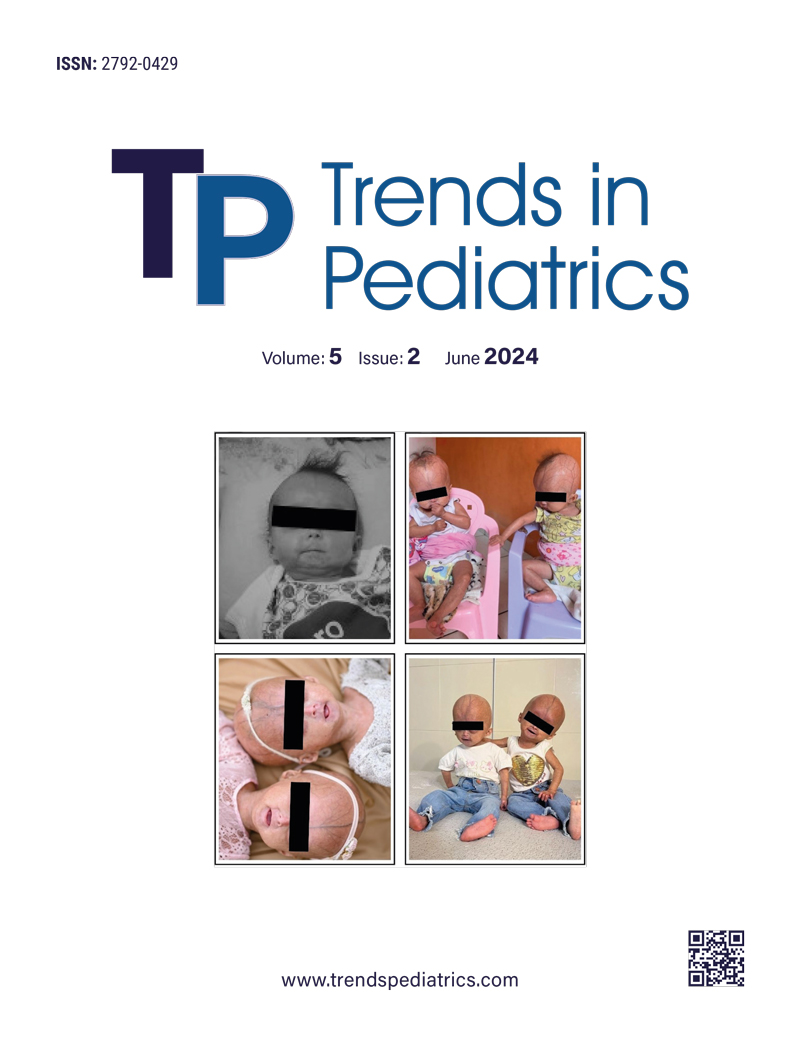
Hutchinson-Gilford Progeria Syndrome (HGPS) is a rare genetic condition characterized by premature aging resulting from an autosomal mutation in the LMNA gene. This article presents a groundbreaking instance of the first female monozygotic twins affected by HGPS, originating from Brazil, highlighting the exceptional nature of this case.
Keywords: Hutchinson-Gilford Progeria syndrome, Monozygotic Twins, female, Progeria
References
- Ahmed MS, Ikram S, Bibi N, Mir A. Hutchinson-Gilford Progeria Syndrome: A Premature Aging Disease. Mol Neurobiol. 2018;55:4417-27. https://doi.org/10.1007/s12035-017-0610-7
- Lamis A, Siddiqui SW, Ashok T, Patni N, Fatima M, Aneef AN. Hutchinson-Gilford Progeria Syndrome: A Literature Review. Cureus. 2022;14:e28629. https://doi.org/10.7759/cureus.28629
- Lima LL, Ribas CBR, Pereira PMR, Eiras JC, Ribas CBR, Schettini RA. Do you know this syndrome? An Bras Dermatol. 2011;86:165-6. https://doi.org/10.1590/s0365-05962011000100031
- The Progeria Research Foundation. 2023. Available at: https://www.progeriaresearch.org (Accessed on June 15, 2023).
- Viégas J, Souza PL, Salzano FM. Progeria in twins. J Med Genet. 1974;11:384-6. https://doi.org/10.1136/jmg.11.4.384
- Dhillon S. Lonafarnib: First Approval. Drugs. 2021;81:283-9. https://doi.org/10.1007/s40265-020-01464-z
- Eriksson M, Brown WT, Gordon LB, et al. Recurrent de novo point mutations in lamin A cause Hutchinson-Gilford progeria syndrome. Nature. 2003;423:293-8. https://doi.org/10.1038/nature01629
- Kamenisch Y, Berneburg M. Progeroid syndromes and UV-induced oxidative DNA damage. J Investig Dermatol Symp Proc. 2009;14:8-14. https://doi.org/10.1038/jidsymp.2009.6
- Misteli T. Farnesyltransferase inhibition in HGPS. Cell. 2021;184:293. https://doi.org/10.1016/j.cell.2020.12.029
- Strandgren C, Revêchon G, Sola-Carvajal A, Eriksson M. Emerging candidate treatment strategies for Hutchinson-Gilford progeria syndrome. Biochem Soc Trans. 2017;45:1279-93. https://doi.org/10.1042/BST20170141
- Solan TD, Lindow SW. Mercury exposure in pregnancy: a review. J Perinat Med. 2014;42:725-9. https://doi.org/10.1515/jpm-2013-0349
- Khan F, Momtaz S, Abdollahi M. The relationship between mercury exposure and epigenetic alterations regarding human health, risk assessment and diagnostic strategies. J Trace Elem Med Biol. 2019;52:37-47. https://doi.org/10.1016/j.jtemb.2018.11.006
Copyright and license
Copyright © 1970 The author(s). This is an open-access article published by Aydın Pediatric Society under the terms of the Creative Commons Attribution License (CC BY) which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.