Abstract
Lymphoma represents a common type of cancer among pediatric populations, exhibiting a range of identifiable symptoms. The aim of this study is to present a case involving a 10-year-old male patient who displayed symptoms of bone pain and arthralgia, ultimately leading to a confirmed diagnosis of B-cell lymphoblastic lymphoma. The patient was admitted to Ali Asghar Hospital in in Tehran, Iran, presenting with complaints of swelling and pain in the right wrist and right ankle that had persisted for six months. Additionally, he developed intermittent fever and bone pain as new symptoms, prompting a series of medical evaluations. Initially, the child was diagnosed with brucellosis, systemic lupus erythematosus, and juvenile idiopathic arthritis six months prior to the final diagnosis of B-cell lymphoblastic lymphoma. Following the commencement of pharmacological treatment, the patient was discharged in stable condition and is currently undergoing chemotherapy.
Keywords: lymphoma, B-cell lymphoblastic, pediatric, case report
INTRODUCTION
Lymphomas are cancers originating from well-developed B and T lymphocytes, often appearing as malignant growths in lymphoid tissues.1
Lymphoma is a frequently occurring type of cancer in children, appearing in different recognizable forms.2 Non-Hodgkin’s lymphoma (NHL) is identified as the fourth most prevalent neoplasm in pediatric populations. In pediatric patients, high-grade histological variants are found in over 90% of NHL instances, in contrast to adults, who predominantly present with low- or intermediate-grade lymphomas.3 NHL encompasses a heterogeneous group of lymphoproliferative disorders that are less clearly defined than Hodgkin lymphomas and exhibit a greater propensity for extranodal dissemination. NHL is classified into four primary categories: diffuse large B-cell lymphoma (DLBCL), which includes primary mediastinal B-cell lymphoma (PMBL), Burkitt lymphoma (BL), lymphoblastic lymphoma (LL), and anaplastic large cell lymphoma (ALCL).2
In the United States, NHL is identified as the seventh most common cancer and the ninth leading cause of cancer-related mortality. NHL constitutes approximately 90% of all lymphoma cases within the country, with its prevalence differing across age demographics; specifically, it represents 62% of lymphoma cases in children aged 0-14 years and 25% in adolescents aged 15-19 years. Furthermore, leukemia accounts for roughly 29% of all cancer diagnoses in the pediatric population.1
Certain B-cell neoplasms may share visual features with BL but have distinct genetic or phenotypic traits. These cases tend to be more aggressive than diffuse large B-cell lymphoma. Pediatric hematologists customize chemotherapy for aggressive B-cell lymphomas based on clinical factors like stage, LDH levels, and bone marrow or CNS involvement rather than histological characteristics.4
Certain signs and symptoms of NHL can include fever, night sweats, weight loss, loss of appetite, and swollen lymph nodes in areas like the neck, axillary, and groin. Lymph nodes may also be visibly enlarged. In some cases, patients may experience symptoms related to areas outside of the lymph nodes, such as gastrointestinal bleeding from stomach lymphoma.5 Common indications include continuous migraines, nausea, increased inflammation and discomfort in the skeletal structure, presence of a growth or accumulation in the abdominal or cervical area, frequent infections, a pale appearance in the eye, queasiness, persistent paleness, changes in eye or vision capabilities, recurrent or prolonged fever with joint inflammation, bleeding gums and nose, as well as swollen eyeballs.6
The aim of this study is to report a case of a 10-year-old boy presenting with symptoms of bone pain and arthralgia, leading to the final diagnosis of B-cell non-Hodgkin lymphoma.
CASE PRESENTATION
A 10-year-old male patient was admitted to Ali Asghar Hospital in Tehran, Iran, presenting with primary complaints of swelling and pain in the right wrist and right ankle that had persisted for six months. Over this period, the symptoms intensified, necessitating the administration of analgesics and the application of a cast. Additionally, the patient developed intermittent fever and bone pain, which prompted further medical interventions. One month prior to the current evaluation, the patient reported experiencing pain in the lower right jaw and observed two nodules on both elbows. Upon examination, vital signs were within normal limits, although swelling was noted in the lower right jaw region. Two nodular masses in both elbows (15*15 mm) were noted without erythema or tenderness. Swelling in multiple joints, including both elbows, right wrist, and right ankle was present. Joints were sensitive to touch and had a limited range of motion. Hepatosplenomegaly was detected on sonography. The initial diagnoses made six months ago for this child were brucellosis, systemic lupus erythematosus (SLE), and juvenile idiopathic arthritis (JIA). Laboratory findings included: WBC: 4500/L (PMN: 41.7%, Lymph: 45.06%, MONO: 10.80%, EO: 10.52%, BA: 0.42%), RBC: 4.02 *10ˆ6 /microL, Hb: 10.3 g/dL, MCV: 77.4 FL, MCH: 25.6 pg, MCHC: 33.1 g/dL, PLT: 183000/mL, ESR: 70, CRP: 40, Wright agglutination: Negative, Coombs Wright: Negative, 2ME: Negative, FANA: Negative, Anti-dsDNA: Negative, ANCA: Negative, Anti-PR3 (C.ANCA): Negative, R.A. Factor: 10 (Negative), VDRL: Non-Reactive, C3, C4, CH50: Normal, LDH: 1540, D-dimer: 4508 ng/dl, CD4/CD8: 0.3%, CD19: 14.9%, CD56: 25.6%.
Right foot MRI showed an Abnormal increase T2/STIR signal intensity in the talus, lateral cuneiform, and tibial epiphysis is noted. Also, a 40×10 mm well-defined T1, T2 lesion was identified at the lateral border of the tibial diaphysis. Mild fusion of the anterior and posterior talus joint and subcutaneous swelling in the lateral and medial ankle were observed. The Right-hand MRI showed without gadolinium (GAD) indicated normal bone structures without destructive processes or signs of osteomyelitis.
Spiral thoracic CT scan with and without contrast showed focal pleural thickening in the posterolateral aspect of the base of right hemothorax, and in visualized cuts of lower neck, a lytic lesion of mandibular body was found. Also, there was a homogenous axillary lymph node with a Short Axis Diameter (SAD) of 16 mm on the right side.
Spiral Abdominopelvic CT scan with and without contrast showed the spleen with a craniocaudal diameter of 165 mm was larger than normal with homogenous parenchymal density. There were multiple homogenous lymphadenopathies in bilateral iliac chains, with a maximum SAD of 21 mm on the left and 15 mm on the right side. Few homogenous paraaortic lymph nodes with SAD up to 6mm and scattered homogenous mesenteric lymphadenopathies with a maximum SAD of 10 mm and retrocrural lymph nodes with SAD of 5 mm were also found.
Spiral Brain CT scan with and without contrast showed mild mucosal thickening of visualized paranasal sinuses was found.
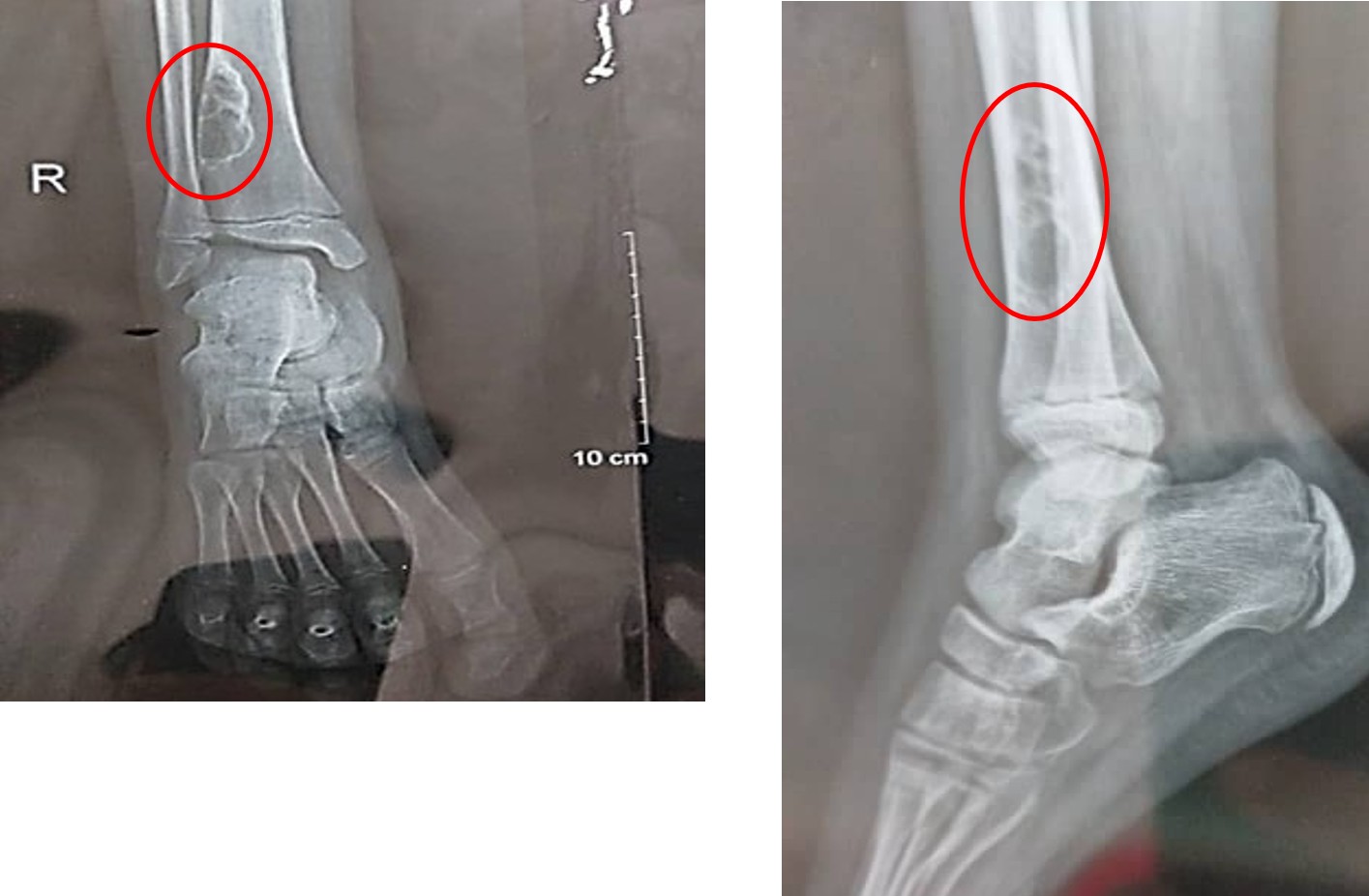
The radiography picture showed the lytic lesions characterized by a permeative appearance were identified in various locations, including the proximal and distal metaphysis of the left humerus, the distal metaphysis of the right humerus, the proximal metaphysis of both sides, the diaphysis of the left ulna, and the distal meta diaphysis of the radius bilaterally. Additionally, a lytic lesion exhibiting a deformed and sclerotic margin, measuring approximately 20×50mm, and situated eccentrically and intracortically, was observed in the lateral aspect of the distal metaphysis of the right tibia (Figure 1).
The sonography pictures showed the suspected lymph nodes (16×15mm) were observed in the right elbow and (14×10mm) in the left elbow. Also, the presence of numerous enlarged pelvic lymph nodes bilaterally, measuring up to 19×27mm on the right side and 25×42mm on the left side, exhibited a highly concerning appearance indicative of potential malignancy infiltration.
A biopsy was conducted on the lymph nodes located in the elbow, specifically from the epitrochlear region, which ultimately led to the diagnosis of B-cell lymphoblastic lymphoma based on the pathological analysis of the biopsy specimen. The bone marrow aspiration yielded normal results. Considering the clinical findings, which included the involvement of cervical lymph nodes and the epitrochlear region, the condition was classified as stage 3 non-Hodgkin’s lymphoma.
Treatment
Management of the patient prior to the establishment of the main diagnosis of the condition (B-cell lymphoblastic lymphoma), the patient was administered co-trimoxazole and rifampin for a duration of six weeks as part of the treatment for brucellosis. Additionally, he received prednisolone for two weeks in relation to the diagnosis of GIA. Following the diagnosis of B-cell lymphoblastic lymphoma, the patient received a treatment regimen consisting of the BFM 2009 protocol. Following the initiation of pharmacological therapy, the patient was released from the medical facility in a favorable overall state and is presently undergoing treatment with chemotherapeutic agents. Following the initiation of treatment, there was a complete resolution of all lymphadenopathies. Additionally, the patient experienced a total alleviation of joint and bone pain; no active bone lesions were detected in the tibia of the right foot, and the previously identified lytic lesions have transformed into sclerotic areas (Figure 2).

Ethical disclosure
The Ethics Committee of Iran University of Medical Sciences (Tehran, Iran) approved this study, which was performed under the approved guidelines (Ethical code: IR.IUMS.REC.1402.1093). For this case report, informed consent has been obtained, and their parents have been assured that their child’s name will not be included in the article and all their information is confidential.
DISCUSSION
The case report discussed in this document involves a patient displaying symptoms indicative of arthritis who was later diagnosed with non-Hodgkin’s Lymphoma. This case study signifies a significant progression in delivering precise clinical care and treatment for patients presenting with similar clinical symptoms. As with numerous other malignancies, the economic ramifications related to lymphomas can vary considerably.7
In the case study conducted by Delavarian et al., a 6-year-old male was observed to exhibit bilateral gingival swelling in the mandible, along with swelling of the right testicle. Ultimately, he was diagnosed with NHL8 in our study; the child patient presented at the medical facility exhibiting symptoms of swelling and discomfort in the right wrist and right ankle.
In a case study conducted by Chaudhary and Borker, a 3-year-old female patient was admitted to the hospital with severe pain and swelling in her right knee joint, which persisted for three months. Radiographic imaging revealed a notable lytic lesion in the supracondylar region of the right femur, along with pathological fractures and multiple lytic lesions in both femurs. The imaging results did not show any signs of lymphadenopathy or organomegaly. Hematological assessments, including peripheral blood smear analysis and bone marrow examination, returned normal findings. A biopsy of the right supracondylar region confirmed the diagnosis of B-cell precursor lymphoblastic lymphoma. Additionally, a computed tomography scan detected a dense and faint lesion in the left adnexal area, which ultimately contributed to the diagnosis of B-cell lymphoblastic lymphoma.9
In a case study conducted by Fujita et al., a 3-year-old female patient was discharged from the hospital with complaints of pain in the right knee following a previous discharge one month earlier due to pain and swelling in the wrist. The patient exhibited limitations in leg mobility. The initial diagnoses included rheumatism and juvenile idiopathic arthritis, which were established based on observations from a T1-weighted MRI scan that revealed abnormally low signal intensity in the femur, tibia, fibula, and bone marrow of the leg. A subsequent contrast-enhanced T1-weighted MRI indicated enhancement of the synovial contrast and the presence of synovial fluid accumulation in the right ankle joint. Laboratory blood tests indicated a white blood cell count of 40,000/μL, with 66% of these cells identified as blasts, alongside a monoclonal increase in lymphoblasts. As a result, the patient was diagnosed with B-cell progenitor acute lymphoblastic leukemia.10
In a study conducted by Marina Boushra, a case report is presented regarding a 2-year-old female diagnosed with isolated torticollis who underwent multiple evaluations in the emergency department and outpatient clinic. During the first three visits, the patient exhibited no associated neurological abnormalities. He was discharged with supportive therapeutic treatment and a probable diagnosis of viral lymphadenitis. Notable findings included swelling of the right wrist and left foot, along with a lytic lesion observed in the initial radiograph of the right ulna. An iliac biopsy yielded non-diagnostic results. On the second day of hospitalization, the patient developed a scalp rash. Subsequent biopsy and flow cytometry of the nodules were consistent with B-cell lymphoblastic lymphoma.11
In a case study conducted by Yan et al., the authors documented a primary lymphoma of the bone localized in the tibial epiphysis, which initially manifested as knee pain. Diagnostic imaging techniques, including X-ray, MRI, CT, and PET-CT, were utilized, followed by a bone biopsy that confirmed the presence of diffuse B-cell lymphoma. Additionally, the patient exhibited a concurrent lesion in the left iliac bone, which upon biopsy, was also identified as diffuse large B-cell lymphoma.12
Compression of the spinal cord caused by NHL is a rare event, as evidenced by a study conducted by Acquaviva et al., the research documented a case involving a 5-year-old female patient who initially complained of pain, which progressed to hyposthenia and post-traumatic paraplegia. Imaging examinations revealed that the compression spanned from the T2 to L4 vertebrae, completely occupying the vertebral canal and extending into the surrounding soft tissues. An emergency surgical procedure was performed, leading to swift tumor regression and eventual full recovery of the patient 42 months after the initial diagnosis. The authors recommend a neurosurgical intervention only in cases where symptoms deteriorate rapidly or for diagnostic purposes, as chemotherapy has shown efficacy in managing such instances.13
In a case study carried out by Ishizuka et al., a 14-year-old female patient presenting with a palpable mass in her right breast was diagnosed with B-lymphoblastic lymphoma at stage I, as determined by immunohistochemical analysis and flow cytometric evaluation.14
In a separate case study conducted by Al Masroori et al., a 5-year-old male patient was admitted to the hospital with symptoms of right knee arthritis and left ankle pain. The patient did not exhibit lymphadenopathy, organomegaly, skin rash, or fever. He experienced difficulty bearing weight and nocturnal pain, initially diagnosed as Juvenile Idiopathic Arthritis. Subsequent bone biopsy of the left femur revealed marrow infiltration by immature blasts. Further diagnostic tests, including blood film analysis, bone marrow aspiration, and flow cytometry indicated 66% blasts with characteristics consistent with B cell progenitors, leading to a final diagnosis of acute lymphoblastic leukemia with B immunophenotype.15
CONCLUSION
According to the description given, B-cell lymphoblastic lymphoma is the predominant malignant hematologic disorder globally, manifesting in diverse recognizable manifestations as outlined, and some patients may present with extranodal involvement. Based on the provided information, the confirmation of B-cell lymphoblastic lymphoma in pediatric patients (particularly pediatric patients presenting with symptoms of joint pain and inflammation) necessitates thorough examination and accurate analysis of laboratory and imaging findings to establish a definitive diagnosis and treatment plan.
Acknowledgements
The authors are grateful to the office of the vice-chancellor and for the research and the support of this study from the Ali Asghar Children’s Superspeciality Training Center of Iran University of Medical Sciences, Tehran, Iran.
Ethical approval
This study has been approved by the Iran University of Medical Sciences (approval date 03.02.2024, number IR.IUMS.REC.1402.1093). Written informed consent was obtained from the participant.
Source of funding
This research has been supported by Iran University of Medical Sciences (Grant number: 27881).
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Bispo JAB, Pinheiro PS, Kobetz EK. Epidemiology and Etiology of Leukemia and Lymphoma. Cold Spring Harb Perspect Med. 2020;10:a034819. https://doi.org/10.1101/cshperspect.a034819
- Thandra KC, Barsouk A, Saginala K, Padala SA, Barsouk A, Rawla P. Epidemiology of non-Hodgkin's lymphoma. Med Sci (Basel). 2021;9:5. https://doi.org/10.3390/medsci9010005
- Buzer WS, Alshwitter NAA, Alorify EM, et al. Pediatric lymphoma incidence at children's hospital Benghazi from 2014 to 2023. International Journal of Science and Research Archive. 2024;11:152-60. https://doi.org/10.30574/ijsra.2024.11.2.0402
- Olszewski AJ, Kurt H, Evens AM. Defining and treating high-grade B-cell lymphoma, NOS. Blood. 2022;140:943-54. https://doi.org/10.1182/blood.2020008374
- Dehghani M, Haddadi S, Vojdani R. Signs, symptoms and complications of non-hodgkin's lymphoma according to grade and stage in South Iran. Asian Pac J Cancer Prev. 2015;16:3551-7. https://doi.org/10.7314/apjcp.2015.16.8.3551
- Mayo Clinic. Non-Hodgkin's lymphoma-symptoms and causes. 2023. Available at: https://wwwmayoclinicorg/diseases-conditions/non-hodgkins-lymphoma/symptoms-causes/syc-20375680.
- Shen Z, Tan Z, Ge L, et al. The global burden of lymphoma: estimates from the Global Burden of Disease 2019 study. Public Health. 2024;226:199-206. https://doi.org/10.1016/j.puhe.2023.11.023
- Delavarian Z, Pakfetrat A, Badiee Z, Ghazi A, Taghizadeh A. Extranodal non-Hodgkin's lymphoma of the oral cavity presenting as gingival swelling: a case report. International Journal of Pediatrics. 2020;8:11537-42.
- Chaudhary N, Borker A. Pediatric precursor B-cell lymphoblastic lymphoma presenting with extensive skeletal lesions. Ann Med Health Sci Res. 2013;3:262-4. https://doi.org/10.4103/2141-9248.113673
- Fujita Y, Kuwashima S, Kato T, et al. Magnetic resonance imaging of a pediatric case of arthritis associated with acute lymphoblastic leukemia: a case report. Exp Ther Med. 2022;24:624. https://doi.org/10.3892/etm.2022.11561
- Boushra M. A case report of B-cell lymphoblastic leukemia/lymphoma presenting as isolated torticollis in a 2-year-old female. Clin Pract Cases Emerg Med. 2020;4:603-6. https://doi.org/10.5811/cpcem.2020.8.48524
- Yan JJ, Chou AJ, Giulino-Roth L, Pomeranz CB. Pediatric primary lymphoma of bone in epiphysis case report. Skeletal Radiol. 2024;53:401-6. https://doi.org/10.1007/s00256-023-04411-7
- Acquaviva A, Marconcini S, Municchi G, Vallone I, Palma L. Non-Hodgkin lymphoma in a child presenting with acute paraplegia: a case report. Pediatr Hematol Oncol. 2003;20:245-51.
- Ishizuka Y, Horimoto Y, Fujimura J, et al. Primary breast non-Hodgkin's lymphoma in a 14-year-old girl: a case report. Surg Case Rep. 2020;6:87. https://doi.org/10.1186/s40792-020-00850-9
- Al Masroori E, Al Hadhrami S, Al Shamli N. Childhood leukemia presenting as clinical arthritis and Chronic Recurrent Multifocal Osteomyelitis (CRMO): case report. Oman Medical Journal. 2023. https://doi.org/10.5001/omj.2025.12
Copyright and license
Copyright © 2025 The author(s). This is an open-access article published by Aydın Pediatric Society under the terms of the Creative Commons Attribution License (CC BY) which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.