Abstract
Objective: Trauma is defined as a life-threatening condition and the leading cause of death in children. The present study aimed to investigate the relationship between clinical findings documented at admission and the interventions implemented in relation to patient outcomes, with the goal of determining the benefits of multidisciplinary treatment in a pediatric intensive care unit (PICU) for patients with trauma.
Method: A retrospective single-center study was conducted, including patients aged 1 month to 18 years who were treated for trauma between March and September 2022 in the PICU. The demographic characteristics, traumatic brain injury/multi-traumas, length of stay, Pediatric Risk of Mortality Score III (PRISM III), neurological findings, laboratories, radiological imaging, mortality, and outcomes were evaluated. Pediatric Trauma Score (PTS), Shock Index (SI), and Shock Index Pediatric Adjusted (SIPA) were calculated. These scores are evaluated for length of stay, transfusions, head injury, and mortality. In addition, the Vasoactive Intotropic Score (VIS), Rotterdam Computed Tomography Score (RCTS), and Functional Status Scale (FSS) were analysed to determine outcomes and effect on mortality.
Results: This study included 55 patients with a mean age of 73.95 (IQR:63.00) months. The mean PRISM III score was 24.95 (IQR:14.00) and the length of stay was 13.27 (IQR: 4.00) days. The most prevalent type of injury was falls from a height, accounting for 47.3% of cases. Furthermore, 28 subjects (50.9%) exhibited brain trauma, while a total of 30 subjects (54.5%) had multiple injuries. Surgery was performed on 21 (38.2%) cases. The mortality rate was 12 (21.8%). The requirement for inotropes (p=0.001), transfusions (p=0.004), and abnormal findings in brain computed tomography (CT) (p=0.036) have been demonstrated to have a significant impact on mortality, with intracranial hemorrhage having a substantial effect on the sequelae (p=0.019). In patients exhibiting elevated risk scores for predicting mortality and protracted PICU admission, PTS (p=0.001; p=0.001), SI (p=0.001; p=0.022), and SIPA (p<0.001; p<0.001) were identified as statistically significant. Despite the absence of a statistically significant relationship between the presence of head trauma and high risk (p>0.05), the need for transfusion was found to be associated with high SIPA (p=0.013). A positive and statistically significant correlation was identified between VIS (r= 0.914), RCTS (r= 0.751), and FSS (r= 0.946) and mortality (p<0.001).
Conclusion: The study demonstrates a statistically significant correlation between PTS, SIPA, VIS, RCTS, FSS, and mortality, as well as length of stay and outcomes. Children who have suffered a serious traumatic injury must be examined using age-based evaluation systems in a timely manner and be transferred to centres that can provide them with appropriate treatment as soon as possible.
Keywords: trauma, children, mortality, intensive care, outcome
INTRODUCTION
Trauma is a considerable and life-threatening condition that is the most common cause of mortality and morbidity in pediatric ages.1-4 Trauma can be classified into four types: physical, chemical, psychological, and thermal. In Turkey, traffic accidents are the leading cause of mortality among children; however, it is important to note that these incidents are preventable.3,5,6 Physical trauma represents a significant health concern, particularly in children over the age of one year. The mechanisms by which these traumas are realized determine the primary risk factors and may result in multiple traumas in children. The increasing mortality and morbidity rates associated with multi-trauma cases are a matter of particular concern. To mitigate the adverse consequences of such traumas, patients must be managed in specialised trauma centers.7,8 It is crucial to meticulously monitor these seriously unwell children in the pediatric intensive care units (PICU) both before and after surgery to avoid complications.
The severity of the trauma and multisystem involvement are the primary determinants of mortality in children who have experienced trauma. In addition to the severity of the trauma, the duration of exposure, the time to access treatment, and the effectiveness of the treatment all have a role. Due to their physiology, children develop shock clinic earlier than adults. The survival probability increases with early intervention, rapid stabilisation, and treatment in a facility equipped with trauma teams. In addition to new imaging techniques, the advantages of being able to perform emergency surgical and interventional procedures quickly when necessary, as well as easily obtaining medicines, supplies, and blood products, are significant.
In our study, we evaluate demographic data and clinical, laboratory, and imaging methods used in the follow-up and treatment of trauma patients in our PICU. The objective of the study was to determine the status of consultation and surgery, the duration of intensive care stay, the need for respiratory support and mechanical ventilation, the requirement for inotropic agents and blood products, mortality and morbidity, and short-term outcomes. For predicting outcomes in pediatric trauma, the Pediatric Trauma Score (PTS), Shock Index (SI), and Shock Index Pediatric Adjusted (SIPA) were used to categorize patients as high risk or low risk based on clinical findings at the time of admission. These scores were evaluated for length of stay, transfusions, head injury, and mortality. In addition, the inotropic using score, Vasoactive Inotropic Score (VIS), was calculated, along with radiological results for the Rotterdam Computed Tomography Score (RCTS) and clinical evaluations for Functional Status Scale (FSS) scores. The relationship between these scores and mortality was evaluated.
Furthermore, the study investigated the success rate of therapy in accordance with the guidelines, utilising data from our center. The hospital is situated in a socioeconomically and culturally disadvantaged region, but it is a tertiary treatment center that offers pediatric intensive care and also features surgical units. In addition to the effect of reaching the trauma center and the initial trauma, the impact of starting early and effective treatment on this situation has also been investigated. The follow-up of PICU-based pediatric trauma patients was investigated with a multidisciplinary approach.
MATERIALS AND METHODS
We conducted a retrospective, single-center study of pediatric patients aged 1 month to 18 years who were admitted to the pediatric intensive care unit (PICU) with trauma between March and September 2022. The study was conducted in a tertiary-care referral hospital with 800 beds and a 52-bed PICU that admits approximately 1,400 patients annually, providing comprehensive surgical services.
Demographic characteristics, type of trauma, indication for PICU admission, past medical history, comorbidities, presence of traumatic brain injury or polytrauma, length of PICU stay, Glasgow Coma Scale (GCS) score, Pediatric Risk of Mortality III (PRISM III) score, pupillary reactivity, occurrence of brain death, post-resuscitation status, need for invasive mechanical ventilation, laboratory and radiologic findings, in-hospital morbidities, and mortality were obtained from electronic medical records. The Pediatric Trauma Score (PTS), Shock Index (SI), and Shock Index Pediatric Age–adjusted (SIPA) were calculated from admission data and analyzed in relation to length of stay, transfusion requirements, head injury, and mortality. In addition, vasoactive-inotropic score (VIS), revised computed tomography score (RCTS), and functional status scale (FSS) were evaluated to assess clinical outcomes.
Vital signs have long been used to predict outcomes in trauma patients, although the prognostic value of systolic blood pressure (SBP), heart rate (HR), and respiratory rate (RR) alone is limited. The SI, defined as HR/SBP, and the SIPA, an age-adjusted modification of the SI, have been investigated as outcome predictors in children. High-risk thresholds are generally defined as SI >0.9 for all ages and SIPA >1.2 for ages 1–6 years, >1.0 for ages 7–12 years, and >0.9 for adolescents. The PTS, based on six clinical parameters, was among the first tools developed and demonstrated high sensitivity and specificity for triage purposes, whereas SIPA has more recently been shown to identify severely injured children with moderate accuracy.
The VIS, which integrates the doses of dopamine, dobutamine, adrenaline, noradrenaline, milrinone, and vasopressin, was calculated as previously described.9 Initially developed to quantify the intensity of vasoactive support in children after congenital cardiac surgery, VIS has been validated as a predictor of adverse outcomes and was applied in this study to critically ill pediatric patients beyond the postoperative cardiac setting.
In children with traumatic brain injury (TBI), the RCTS evaluates radiologic findings, including the status of basal cisterns, presence of midline shift, epidural mass lesion, intraventricular hemorrhage, and subarachnoid hemorrhage.10 The total score reflects the severity of cranial injury and stratifies mortality risk in moderate-to-severe TBI. Higher RCTS values are associated with increased mortality and worse functional outcomes, whereas lower scores are correlated with improved survival.
Because mortality alone does not fully capture clinical outcomes in pediatric trauma, functional morbidity was also assessed. The FSS was developed through a consensus process among pediatric health professionals to standardize the evaluation of long-term sequelae.11 It measures six domains—mental status, sensory function, communication, motor function, feeding, and respiratory status—with scores ranging from 6 to 30, where lower scores indicate better function.
In accordance with current guidelines, prophylactic antiepileptic therapy was initiated in patients with TBI and a GCS score <8. Levetiracetam was administered intravenously at a dose of 20 mg/kg/day. Antiepileptic treatment was also initiated in patients with a history of cardiopulmonary resuscitation or in those who developed new seizures. For patients presenting with active seizures, intravenous midazolam (1–2 mg/kg per dose) was given as a loading treatment, followed by intravenous levetiracetam at 20 mg/kg/day.
All patients were managed in the PICU under the supervision of pediatric intensive care specialists with continuous monitoring. Multidisciplinary consultations were obtained as needed for comprehensive evaluation and organ-specific management. Patients requiring urgent surgical or minimally invasive intervention upon presentation to the emergency department were stabilized post-procedure and subsequently admitted to the PICU for further care. Treatments were continued in the PICU both before and after definitive interventions. Neurosurgery, pediatric surgery, orthopedics, plastic and reconstructive surgery, otolaryngology, and pediatric neurology teams were actively involved in the management of these patients.
Patient data were extracted from electronic medical records and entered into a standardized database. Before study initiation, ethical approval was obtained from the institutional ethics committee (HRÜ/22.18.04), in accordance with the principles of the Declaration of Helsinki.
Statistical analyses were performed using SPSS software (IBM SPSS Statistics for Windows, version 26.0; IBM Corp., Armonk, NY, USA). The normality of distribution was assessed with the Kolmogorov–Smirnov test. Continuous variables are presented as mean ± standard deviation (SD) when normally distributed, and as median with interquartile range (IQR) when non-normally distributed. Categorical variables are expressed as frequencies and percentages. Comparisons of categorical variables were made using Pearson’s chi-square test or Fisher’s exact test, as appropriate. Correlations between continuous variables were examined with Pearson’s correlation analysis. To determine the factors influencing the mortality status of patients included in the study, multiple regression analysis was performed. A two-tailed p-value <0.05 was considered statistically significant.
RESULTS
A total of 55 pediatric patients with trauma were included in the study, of whom 38 (69.1%) were male and 17 (30.9%) female. The median age was 74 months (IQR, 63). The mean PRISM III score at admission was 24.9 (IQR, 14), and the median length of PICU stay was 13 days (IQR, 4).
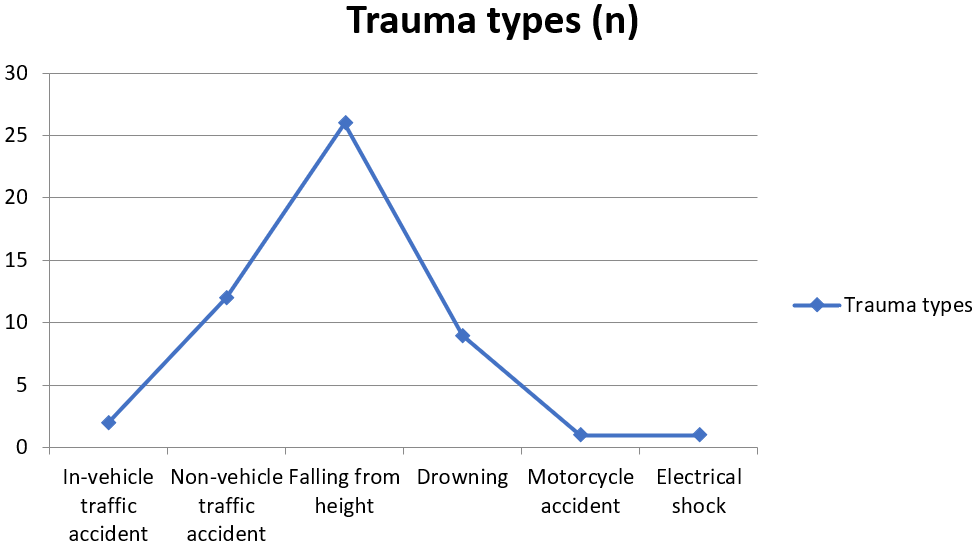
Falls from height were the most common cause of trauma (n=26, 47.3%), followed by traffic accidents and other mechanisms (Figure 1). The highest rate of admissions occurred in June (23.6%). Twenty-eight patients (50.9%) sustained traumatic brain injury, and 30 (54.5%) had multiple injuries involving other organs or systems. Twenty-one patients (38.2%) underwent surgery, most commonly neurosurgical (n=18, 85.7%) or pediatric surgical procedures (n=6, 28.6%). The majority of patients (n=53, 96.4%) had no significant comorbidities.
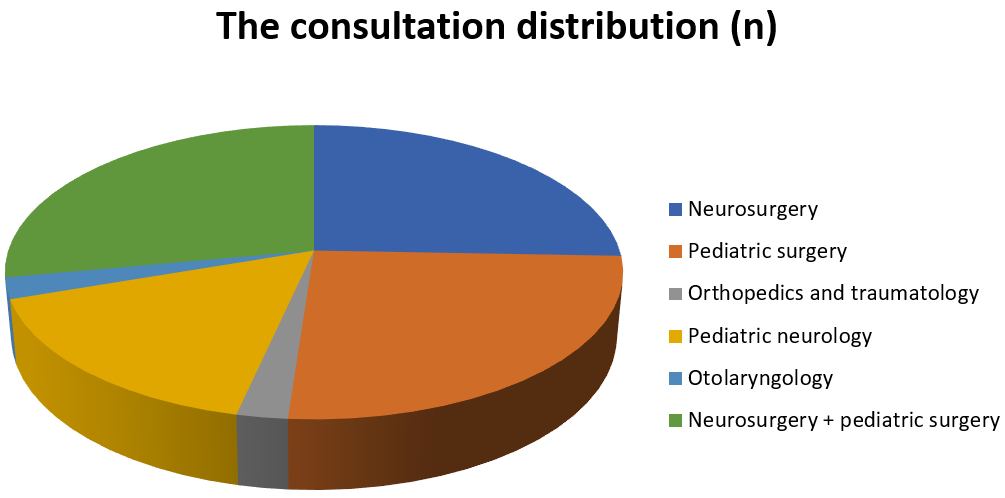
At presentation, 23 patients (41.8%) had a GCS score <8, 11 (20.0%) lacked pupillary light reflex, 15 (27.3%) required cardiopulmonary resuscitation, and 9 (16.4%) had clinical signs of brain death. Most patients were admitted to the PICU after initial stabilization in the emergency department (n=30, 54.5%). During the PICU stay, 21 patients (38.2%) did not require respiratory support, 41 (74.5%) required inotropic therapy, and 19 (34.5%) received blood or blood product transfusion (Table 1). Multidisciplinary management was provided with consultations from neurosurgery, pediatric surgery, orthopedics and traumatology, otolaryngology, and pediatric neurology (Figure 2). Pathological findings on initial radiologic examinations are summarized in Table 2.
| Table 1. The distribution of transfusion types and intracranial traumas | ||
|
|
||
| Transfusion types | None |
|
| Erythrocyte suspension |
|
|
| Platelet suspension |
|
|
| Fresh frozen plasma |
|
|
| Erythrocyte & Platelet suspension |
|
|
| Erythrocyte suspension & Fresh frozen plasma |
|
|
| Erythrocyte & Platelet suspension & Fresh frozen plasma |
|
|
| Intracranial traumas | Normal |
|
| Epidural hemorrhage |
|
|
| Subdural hemorrhage |
|
|
| Subaracnoidal hemorrhage |
|
|
| Intraparenchymal hemorrhage |
|
|
| Diffuse parancimal edema |
|
|
| *PAAG: posteroanterior chest X-ray, CT: Computed tomography | ||
| Table 2. Radiological findings | ||
| Radiological imagings | Findings |
|
| PAAG* | Normal |
|
| Pathological findings (pneumothorax, hemothorax) |
|
|
| Cranial CT* | Normal |
|
| Intracranial hemorrhage |
|
|
| Diffuse parenchymal edema |
|
|
| Collapse fracture |
|
|
| Thorax CT* | Normal |
|
| Pathological findings (pneumothorax, hemothorax) |
|
|
| Abdomen CT* | Normal |
|
| Pathological findings (perforation, hemorrhage) |
|
|
Twelve patients (21.8%) died during their PICU stay. Of the survivors, 43 (74.5%) were discharged to pediatric wards, and 2 (3.6%) were discharged to the palliative care unit. Prophylactic antiepileptic medication was administered to 23 patients (41.8%), and seizure therapy was required in 3 (5.5%). At discharge, four patients (7.3%) required nasogastric tube feeding, 2 (3.6%) had tracheostomies with home ventilator support, and central nervous system (CNS) sequelae were documented in 3 (7%).
No significant associations were observed between month of trauma (p=0.942), trauma type (p=0.471), or the presence of brain trauma (p=0.217), multiple trauma (p=0.436), or surgical intervention (p=0.288) and mortality. In contrast, the need for inotropic support (p=0.001), transfusion of blood products (p=0.004), and abnormal cranial CT findings (p=0.036) were significantly associated with increased mortality. Although brain trauma and surgical intervention were not significantly correlated (p=0.066), the presence of intracranial hemorrhage on CT was significantly associated with the development of CNS sequelae (p=0.019).
High-risk scores on the Pediatric Trauma Score (PTS), Shock Index (SI), and Shock Index Pediatric Age–adjusted (SIPA) were significantly associated with both mortality (PTS, p=0.001; SI, p=0.001; SIPA, p<0.001) and prolonged PICU stay (PTS, p=0.001; SI, p=0.022; SIPA, p<0.001) (Table 3). There was no significant association between the presence of head trauma and high-risk scores (p>0.05). However, the need for transfusion was significantly associated with high SIPA scores (p=0.013). In contrast, when cranial pathologies and transfusion types were analyzed separately, no significant relationships were observed (p>0.05).
| * PTS: Pediatric Trauma Score, SI: Shock Index, SIPA: Shock Index Pediatric Adjusted | |||||||
| Table 3. Distribution of SI, SIPA, and PTS at the time of admission, and these high and low-risk scores for the length of stay, transfusions, head injury, and mortality relationships | |||||||
|
|
|
|
|||||
|
|
|
|
|
|
|
||
| Mortality (n) | No |
|
|
|
|
|
|
| Yes |
|
|
|
|
|
|
|
| p value |
|
|
|
||||
| Intracranial pathology (n) | Normal |
|
|
|
|
|
|
| p value |
|
|
|
||||
| Epidural hemorrhage |
|
|
|
|
|
|
|
| p value |
|
|
|
||||
| Subdural hemorrhage |
|
|
|
|
|
|
|
| p value |
|
|
|
||||
| Sub-arachnoidal hemorrhage |
|
|
|
|
|
|
|
| p value |
|
|
|
||||
| Intra-parancimal hemorrhage |
|
|
|
|
|
|
|
| p value |
|
|
|
||||
| Diffuse edema |
|
|
|
|
|
|
|
| p value |
|
|
|
||||
| Transfusion types (n) | None |
|
|
|
|
|
|
| p value |
|
|
|
||||
| Erythrocyte suspension |
|
|
|
|
|
|
|
| p value |
|
|
|
||||
| Platelet suspension |
|
|
|
|
|
|
|
| p value |
|
|
|
||||
| Fresh frozen plasma |
|
|
|
|
|
|
|
| p value |
|
|
|
||||
| Erythrocyte & Platelet suspension |
|
|
|
|
|
|
|
| p value |
|
|
|
||||
| Erythrocyte suspension & Fresh frozen plasma |
|
|
|
|
|
|
|
| p value |
|
|
|
||||
| Erythrocyte & Platelet suspension & Fresh frozen plasma |
|
|
|
|
|
|
|
| p value |
|
|
|
||||
| Length of stay (day) | Median (IQR) |
|
|
|
|
|
|
| p value |
|
|
|
||||
Among patients with critical trauma, VIS scores ranged from 0 to 220 (median, 0). RCTS values based on cranial CT findings ranged from 1 to 6 (median, 1). Functional assessment of survivors yielded FSS scores ranging from 1 to 30 (median, 6). Multiple regression analysis revealed that VIS (r=0.914, p<0.001), RCTS (r=0.751, p<0.001), and FSS (r=0.946, p<0.001) were independently and significantly associated with mortality, indicating that each parameter contributed as a strong predictor of adverse outcomes beyond the effects of the others.
DISCUSSION
Trauma is reported as the second most frequent cause of death among children aged 1-4 years after infections from underdeveloped and developing countries. It is the most common cause of death in developed countries for those aged 1 to 14.8,12 Physical traumas in childhood increase mortality, morbidity, and health expenditures in countries. As observed in our study, in research examining childhood traumas in Turkey, Öztan et al. (2-11) found that 0.5-17 (6.3) years was the age range of children with trauma.13 Tambay et al. reported a mean hospital stay of 5.54 ± 6.42 days, while Mısırlıoğlu et al. recorded an average of 11.8 ± 8.2 days. The mean duration of PICU stay was 4.4 ± 2.9 days.7,14 While the majority of trauma patients were found to be healthy in this study, the period of hospitalization in the PICU was found to be longer than in other studies. This is likely due to the fact that the hospital is the only pediatric trauma center in the city and has high PRISM III scores.
Falling from height is the most common cause of trauma in all age groups following motor vehicle accidents, and it is the most prevalent cause of trauma in childhood.15 Similar to the literature, falling from a height was the most often cause of trauma in this study. The month of June, which corresponds with the commencement of the school holidays in this country, exhibits a marked increase in the number of trauma patients, attributable to the warming of the weather. This month is thus identified as the most significant month in terms of trauma admissions in our study.
Head trauma and/or brain injury are the most common form of pediatric trauma and are the most common cause of trauma-related mortality and morbidity.16 Doğan et al. in their study of pediatric traumas found that the most common region was the head and neck region, with a rate of 41.9%. Extremity traumas were observed in 33.4% of cases.17 The present study provides support for these rates, and it was found that the rate of consultation with neurosurgeons and pediatric surgeons was higher than that of other specialists.
It is known that 30-50% of trauma-related deaths occur at the accident site, and 30% of them occur in the hours and days after the accident, usually in the first hours.18 The high PRISM III scores of the patients included in the study, which evaluates the data of the first 24 hours of PICU admission, the presence of a high rate of head trauma, and the high rate of multiple trauma, describe the fact that the mortality rate is higher compared to literature data. Mortality rates can be reduced by prompt recognition of patients who require appropriate and rapid transport, urgent evaluation and resuscitation, and necessary surgical intervention. In addition, it is essential to reduce mortality and morbidity through effective management, treatment, and a multidisciplinary approach in pediatric emergency care and the PICU.
In the study by Embleton et al., only traffic accident traumas were examined, with a mean age/gender of 11.2 years/60.1% male, respectively. Accidents occurred at 45.6% in the summer, the mortality rate was 3.8%, and CNS sequelae were 1.9% reported.19 In the PICU treatment study, Misirlioglu et al. followed up and treated 49 pediatric trauma patients, but no mortality was detected during this process.14 On the contrary, at the end of our study, the mortality rate was higher, and it was associated with patients’ first clinical scores at admission. This underscores the significance of scoring systems such as the SI, SIPA, and PTS, which are utilized in the preliminary assessment of critically ill trauma patients, in predicting mortality. Additionally, we examined 55 patients over only 6 months. The high rate is due to the high number of pediatric patients in our region and the high incidence of physical trauma because of weak socioeconomic and sociocultural conditions. Additionally, our facility is the only trauma center in the region with a pediatric intensive care physician. Our patients, unlike other study results, showed a newly developed high rate of central nervous and respiratory system support needs at the end of the study. This situation is associated with the severity of the primary trauma etiology of our patients and the high rate of patients with severe shock in the clinic. This condition shows that the duration of hypoxemic and hypotensive stay is prolonged due to difficulties in reaching our center for various reasons.
In Özcan et al., the factors affecting mortality in pediatric severe TBI study, it was observed that CPR was applied in patients who lost their lives, the need for inotropes and the need for erythrocyte transfusion were statistically significantly higher.20 Our study identified a statistically significant relationship between the necessity for inotropic agent administration and blood product transfusions and the mortality rate. Furthermore, the presence of hemorrhage, diffuse edema, and fractures on brain CT scans was found to have a statistically significant impact on mortality.
In pediatric TBI patients, the most common findings at cranial brain CT imaging are diffuse axonal injury, edema, midline shift, and subdural and intraparenchymal hemorrhage.21 Our critically ill trauma patients had similar rates of pathologies. Interestingly, we detected that while there was no significant relationship between the presence of brain trauma and the need for an operation, the presence of hemorrhage on brain CT significantly affected the development of CNS sequelae. This situation demonstrates the significant impact of primary injury caused by trauma and its severity on mortality and morbidity. Moreover, the higher final mortality rate compared to other studies may be attributed to the sociocultural and socioeconomic weakness of the region where the study was conducted. Additionally, trauma patients took longer to reach our center, and transportation systems were difficult due to physical reasons in our region. There is evidence to suggest that delayed initial treatment of patients can affect their prognosis.
The Injury Severity Score (ISS) is the most commonly utilised injury scoring system in the domains of trauma research and benchmarking. An ISS>15 is conventionally used to define severe injury. In a study by Brown et al., the relationship between ISS scoring and mortality in children was examined. The study suggests that ISS>25 may be a more appropriate definition of severe injury in paediatric trauma patients. However, it is important to note that in paediatric patients with single-system injury, mortality is primarily driven by head and chest injuries. This suggests that the specific pattern of injury may be more significant than the overall ISS score. The assumption that adult injury metrics can be applied to pediatric patients with adequate performance must be robustly evaluated to ensure the best care for the injured child.22 In light of the findings that different scores would be more appropriate than the ISS used in adults, the mortality rate was evaluated with scores such as PTS, SI, and SIPA in the present study. Pediatric outcomes were also examined with FSS.
In a study published in 2023, where 750 pediatric trauma patients were examined retrospectively, predictive outcomes (length of stay, disposition, ventilator use, Index Severity Score, and spleen/liver injury) data of patients with high-risk scores in the PTS and SIPA scoring were analyzed, and odds ratios were associated with increased risk for both scores. When the PTS and SIPA were compared, it was determined that the odds ratio was higher in the PTS, while the need for urgent fluid replacement was higher in the SIPA score.23 In our study, we found that pediatric trauma patients with high-risk scores for predicting mortality and prolonged PICU stay were statistically significant. This finding lends further support to the hypothesis that these scoring systems are effective in predicting length of stay, mortality, and outcomes in paediatric trauma patients.
The American College of Surgeons Pediatric Trauma Quality Improvement Program database compared SIPA scores in patients with and without TBI. Higher blood transfusion requirements and increased mortality rates were found in patients with TBI. Isolated TBI and those with multisystem injury, suggesting its utility in the prediction of outcome in TBI patients with elevated SIPA regardless of the presence of concomitant injuries. For this reason, it has been suggested to develop scoring systems that include the status and severity of TBI in the analysis of trauma patients.24 In our study conducted without isolating TBI, there was no statistically significant relationship between the presence of head trauma and high-risk scores at PTS, SI, and SIPA. Similarly, in those with high-risk SIPA scores, the need for blood transfusion was found to be statistically significantly higher.
The three-year study of pediatric sepsis patients in the PICU examined the association between VIS scores and mortality. In addition to mortality, it was also found to be associated with PICU length of stay, mechanical ventilator days, cardiac arrest, and extracorporeal membrane oxygenation.9 In a study examining sepsis patients in adult intensive care over an 11-year period, the VIS score was calculated at 2-hour intervals for a 72-hour period. Inotrope treatment was evaluated according to the VIS score. The relationship between the VIS score and mortality was examined. The study concluded that the VIS score was both a reliable predictor of 28-day mortality and a valuable tool in clinical decision-making processes within intensive care management.25 Although the VIS score is primarily a predictor of mortality in sepsis and cardiac surgery patients, it has also been shown to be a predictor of mortality in TBI patients in the Adult TBI Study.26 A study on the use of RCTS as a predictor of mortality in pediatric TBI patients found that the use of validated RCTS, especially in patients with moderate or severe TBI, provides accurate data and can be used for risk stratification.10 The FSS is a tool for producing a functional status result at the end of a major intervention. As it provides clear, non-subjective data, it provides standardisation in patient assessment. When evaluated using the Adaptive Behaviour Assessment System (ABAS) II, the study assessing its feasibility and effectiveness reported that it was quick, reliable, and suitable for use in hospitalized pediatric patients.11 This study found a positive and statistically significant correlation between VIS, RCTS, and FSS and mortality, similar to the results of mortality and outcome prediction evaluations reported in the literature.
A retrospective cohort study was published in 2021, using data from 2012 to 2017, and was conducted in 832 emergency departments (EDs) across the United States of America (USA), located in all 50 states and the District of Columbia. The study focused on admission, transfer, or injury-related death at a participating trauma centre. The objective of the study was to evaluate the relationship between pediatric ED preparation, in-hospital mortality, and in-hospital complications in injured children admitted to USA trauma centres. The study compared injured children treated in high-prepared EDs with those treated in low-prepared EDs. The mortality rate was lower in the former group, but no fewer complications were observed.27 This finding underscores the significance of multidisciplinary management of pediatric trauma patients in reducing mortality in centres with teams with expertise in trauma surgery, such as the hospital where our study was conducted.
This study was conducted retrospectively at a single center. Nevertheless, the clinic and interventions for trauma patients during admission to the PICU were performed by the same group of physicians and surgeons. Intracranial pressure and continuous electroencephalography monitoring could not be applied due to a lack of equipment. Although the admission indications and severity of traumas were heterogeneous, this study center was the only pediatric intensive care specialist clinic in this city. Patients with severe or moderate physical traumas were treated in a multidisciplinary manner by a team of neurosurgeons, pediatric surgeons, orthopedists, traumatologists, otolaryngologists, and pediatric neurologists.
CONCLUSION
In conclusion, the results of our single-centre study demonstrate a statistically significant correlation between PTS, SIPA, VIS, RCTS, FSS, and mortality, as well as length of stay and outcomes. These results are analogous to those reported in the literature regarding mortality and outcome prediction evaluations. Children who have suffered a serious traumatic injury should be quickly recognized, examined with clinical findings and age-based evaluation systems/scoring tools, and taken as soon as possible to centers that can provide them with appropriate treatment. Although this study population showed some results, multi-center prospective studies are needed to obtain clear data and develop the first recognition charts and transfer conditions on the management and mortality of pediatric trauma patients.
Ethical approval
This study has been approved by the Harran University Clinical Research Ethics Committee (approval date 19.09.2022, number HRÜ/22.18.04). Written informed consent was obtained from the participants.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Boomer LA, Nielsen JW, Lowell W, et al. Managing moderately injured pediatric patients without immediate surgeon presence: 10 years later. J Pediatr Surg. 2015;50:182-5. https://doi.org/10.1016/j.jpedsurg.2014.10.041
- Fiorentino JA, Molise C, Stach P, et al. Pediatric trauma. Epidemiological study among patients admitted to Hospital de Niños “Ricardo Gutiérrez”. Arch Argent Pediatr. 2015;113:12-20.
- öztürk H, Dokucu AI, Otcu S, Onen A. The prognostic importance of trauma scoring systems for morbidity in children with penetrating abdominal wounds: 17 years of experience. J Pediatr Surg. 2002;37:93-8. https://doi.org/10.1053/jpsu.2002.29436
- Schlegel C, Greeno A, Chen H, et al. Evolution of a level I pediatric trauma center: Changes in injury mechanisms and improved outcomes. Surgery. 2018;163:1173-7. https://doi.org/10.1016/j.surg.2017.10.070
- Sathiyasekaran BW. Accident trauma--a descriptive hospital study. J R Soc Health. 1991;111:10-1. https://doi.org/10.1177/146642409111100104
- Aldinç H, Gün C. Analysis of pediatric traumas characteristics and the role of scoring systems. Bosphorus Med J. 2020;7:11-5. https://doi.org/10.14744/bmj.2019.32932
- Tambay G, Satar S, Kozacı N, Açıkalın A. Retrospective analysis of pediatric trauma cases admitted to the emergency medicine department. Acad Emerg Med. 2013;12:8. https://doi.org/10.5152/jaem.2013.008
- Grinkeviciūte DE, Kevalas R, Saferis V, Matukevicius A, Ragaisis V, Tamasauskas A. Predictive value of scoring system in severe pediatric head injury. Medicina (Kaunas). 2007;43:861-9.
- McIntosh AM, Tong S, Deakyne SJ, Davidson JA, Scott HF. Validation of the Vasoactive-Inotropic Score in Pediatric Sepsis. Pediatr Crit Care Med. 2017;18:750-757. https://doi.org/10.1097/PCC.0000000000001191
- Liesemer K, Riva-Cambrin J, Bennett KS, et al. Use of Rotterdam CT scores for mortality risk stratification in children with traumatic brain injury. Pediatr Crit Care Med. 2014;15:554-62. https://doi.org/10.1097/PCC.0000000000000150
- Pollack MM, Holubkov R, Glass P, et al. Functional Status Scale: new pediatric outcome measure. Pediatrics. 2009;124:e18-28. https://doi.org/10.1542/peds.2008-1987
- Bayrakçı B, Tekşam Ö. Çocuklarda travmaya genel yaklaşım. Katkı Pediatri Dergisi. 2009;31:115-31.
- Öztan MO, Anıl M, Anıl AB, et al. First step toward a better trauma management: Initial results of the Northern Izmir Trauma Registry System for children. Ulus Travma Acil Cerrahi Derg. 2019;25:20-28. https://doi.org/10.5505/tjtes.2018.82780
- Mısırlıoğlu M, Yöntem A, Ekinci F, Horoz ÖÖ. Çocuk yoğun bakım ünitemizde takip edilen travma hastalarının değerlendirilmesi. Pediatr Pract Res. 2019;7:439-45.
- O’Neill JA. Advances in the management of pediatric trauma. Am J Surg. 2000;180:365-9. https://doi.org/10.1016/s0002-9610(00)00488-8
- Melo JRT, Di Rocco F, Lemos-Júnior LP, et al. Defenestration in children younger than 6 years old: mortality predictors in severe head trauma. Childs Nerv Syst. 2009;25:1077-83. https://doi.org/10.1007/s00381-009-0924-5
- Doğan Z, Kukul Güven FM, Cankorkmaz L, Korkmaz L, Coşkun A, Döleş KA. Evaluation of pediatric cases presenting to the emergency department of our hospital because of trauma. Turk Arch Ped. 2011;46:156-60. https://doi.org/10.4274/tpa.46.65
- Serinken M, Ozen M. Characteristics of injuries due to traffic accidents in the pediatric age group. Ulus Travma Acil Cerrahi Derg. 2011;17:243-7. https://doi.org/10.5505/tjtes.2011.13845
- Embleton DB, Ertoran İ, Önen N, Özkan A, Mersin H, Tekeli MC. Mortality and morbidity in children as traffic accident victims. Kocatepe Med J. 2016;17:84-8. https://doi.org/10.18229/kocatepetip.242403
- Özcan S, Bozkurt İ, Akay S, et al. Factors affecting mortality in pediatric severe head injury. Genel Tıp Derg. 2022;32:469-75. https://doi.org/10.54005/geneltip.1160967
- Stopa BM, Dolmans RGF, Broekman MLD, Gormley WB, Mannix R, Izzy S. Hyperosmolar Therapy in Pediatric Severe Traumatic Brain Injury-A Systematic Review. Crit Care Med. 2019;47:e1022-31. https://doi.org/10.1097/CCM.0000000000004003
- Brown JB, Gestring ML, Leeper CM, et al. The value of the injury severity score in pediatric trauma: Time for a new definition of severe injury? J Trauma Acute Care Surg. 2017;82:995-1001. https://doi.org/10.1097/TA.0000000000001440
- Jeong YS, Shah S, Akula S, Novotny N, Menoch M. Pediatric trauma smackdown: PTS vs SIPA. Injury. 2023;54:1297-301. https://doi.org/10.1016/j.injury.2023.02.045
- Reppucci ML, Phillips R, Meier M, et al. Pediatric age-adjusted shock index as a tool for predicting outcomes in children with or without traumatic brain injury. J Trauma Acute Care Surg. 2021;91:856-60. https://doi.org/10.1097/TA.0000000000003208
- Xiao S, Zhuang Q, Li Y, Xue Z. Longitudinal Vasoactive Inotrope Score Trajectories and Their Prognostic Significance in Critically Ill Sepsis Patients: A Retrospective Cohort Analysis. Clin Ther. 2024;46:711-6. https://doi.org/10.1016/j.clinthera.2024.07.006
- Kara I, Sargin M, Bayraktar YS, et al. The Relationship Between Vasoactive-Inotropic Score and Mortality in Adult Patients with Traumatic Brain Injury. Turk Neurosurg. 2019;29:254-61. https://doi.org/10.5137/1019-5149.JTN.25177-18.1
- Newgard CD, Lin A, Olson LM, et al. Evaluation of Emergency Department Pediatric Readiness and Outcomes Among US Trauma Centers. JAMA Pediatr. 2021;175:947-56. https://doi.org/10.1001/jamapediatrics.2021.1319
Copyright and license
Copyright © 2025 The author(s). This is an open-access article published by Aydın Pediatric Society under the terms of the Creative Commons Attribution License (CC BY) which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.