Abstract
The diagnosis of childhood osteoporosis is relatively straightforward in primary bone diseases. However, in chronic diseases that can cause osteoporosis, the focus is often on primary treatment, and the risk of osteoporosis is frequently overlooked. Primary bone disease typically presents in infancy or early childhood with multiple fractures of long bones, abnormalities of the sclera or teeth, and an associated family history. On the other hand, secondary osteoporosis is associated with underlying chronic disease and long-term use of medications for these conditions. It may present with vertebral fractures as the only sign. Clinicians must be vigilant in diagnosing it due to its more insidious course. Once diagnosed, diet and lifestyle changes should be made. Also, any vitamin and mineral deficiencies should be replaced. The next step will be the identification of patients who are suitable for medical treatment. In some cases, patients with multiple bone deformities may require corrective surgery. Children diagnosed with osteoporosis should be monitored by a pediatric bone specialist, and their treatment should be coordinated by a multidisciplinary team.
Keywords: osteoporosis, osteogenesis imperfecta, management, treatment, bisphosphonates
References
- Grover M, Bachrach LK. Osteoporosis in children with chronic illnesses: diagnosis, monitoring, and treatment. Curr Osteoporos Rep. 2017;15:271-82. [Crossref]
- Gordon CM, Zemel BS, Wren TAL, et al. The determinants of peak bone mass. J Pediatr. 2017;180:261-9. [Crossref]
- Al-Bari AA, Al Mamun A. Current advances in regulation of bone homeostasis. FASEB Bioadv. 2020;2:668-79. [Crossref]
- Yaşar E, Adigüzel E, Arslan M, Matthews DJ. Basics of bone metabolism and osteoporosis in common pediatric neuromuscular disabilities. Eur J Paediatr Neurol. 2018;22:17-26. [Crossref]
- Caradonna P, Rigante D. Bone health as a primary target in the pediatric age. Eur Rev Med Pharmacol Sci. 2009;13(2):117-128.
- Vierucci F, Saggese G, Cimaz R. Osteoporosis in childhood. Curr Opin Rheumatol. 2017;29:535-46. [Crossref]
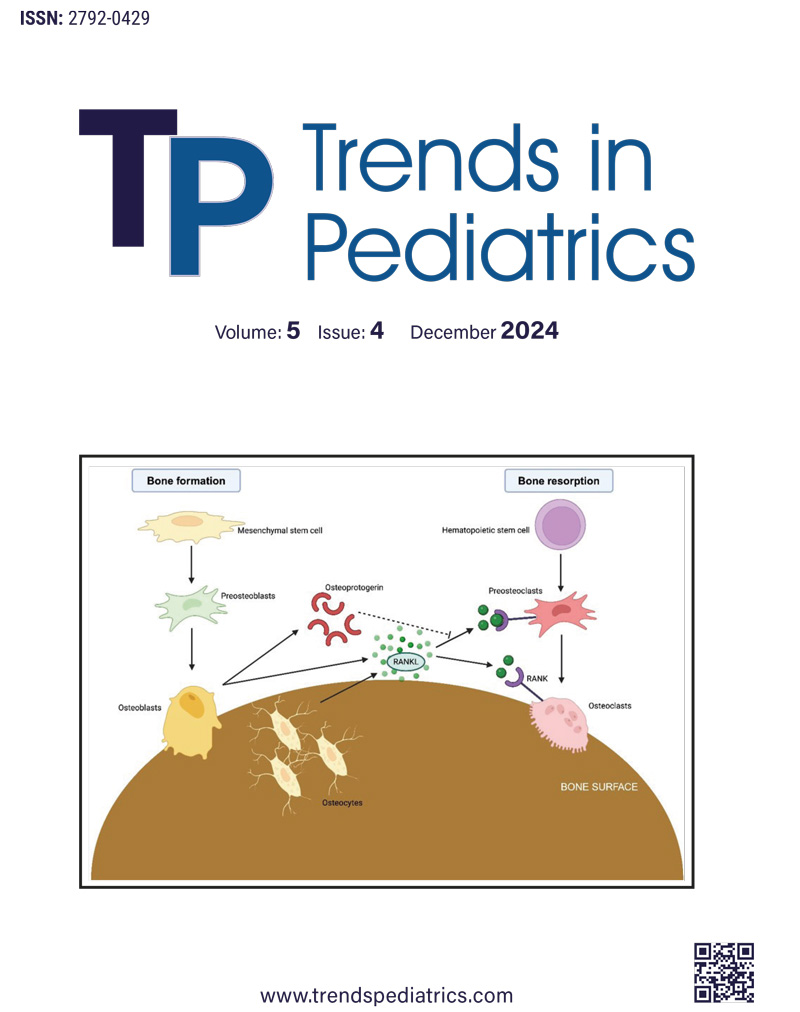
- Boyce BF, Xing L. Functions of RANKL/RANK/OPG in bone modeling and remodeling. Arch Biochem Biophys. 2008;473:139-46. [Crossref]
- Weitzmann MN. The role of inflammatory cytokines, the RANKL/OPG axis, and the immunoskeletal interface in physiological bone turnover and osteoporosis. Scientifica (Cairo). 2013;2013:125705. [Crossref]
- Lim DBN, Moon RJ, Davies JH. Advances in diagnosis and management of childhood osteoporosis. J Clin Res Pediatr Endocrinol. 2022;14:370-84. [Crossref]
- Nampoothiri S, Guillemyn B, Elcioglu N, et al. Ptosis as a unique hallmark for autosomal recessive WNT1-associated osteogenesis imperfecta. Am J Med Genet A. 2019;179:908-14. [Crossref]
- Gao Y, Chen N, Fu Z, Zhang Q. Progress of wnt signaling pathway in osteoporosis. Biomolecules. 2023;13:483. [Crossref]
- Maeda K, Kobayashi Y, Koide M, et al. The regulation of bone metabolism and disorders by wnt signaling. Int J Mol Sci. 2019;20:5525. [Crossref]
- Wu M, Chen G, Li YP. TGF-β and BMP signaling in osteoblast, skeletal development, and bone formation, homeostasis and disease. Bone Res. 2016;4:16009. [Crossref]
- Ciancia S, van Rijn RR, Högler W, et al. Osteoporosis in children and adolescents: when to suspect and how to diagnose it. Eur J Pediatr. 2022;181:2549-61. [Crossref]
- Boyce AM, Gafni RI. Approach to the child with fractures. J Clin Endocrinol Metab. 2011;96:1943-52. [Crossref]
- Steffey CL. Pediatric osteoporosis. Pediatr Rev. 2019;40:259-61. [Crossref]
- Shuhart CR, Yeap SS, Anderson PA, et al. Executive summary of the 2019 ISCD position development conference on monitoring treatment, DXA cross-calibration and least significant change, spinal cord injury, peri-prosthetic and orthopedic bone health, transgender medicine, and pediatrics. J Clin Densitom. 2019;22:453-71. [Crossref]
- Ward LM, Weber DR, Munns CF, Högler W, Zemel BS. A contemporary view of the definition and diagnosis of osteoporosis in children and adolescents. J Clin Endocrinol Metab. 2020;105:dgz294. [Crossref]
- Deguchi M, Tsuji S, Katsura D, Kasahara K, Kimura F, Murakami T. Current overview of osteogenesis imperfecta. Medicina (Kaunas). 2021;57:464. [Crossref]
- Marom R, Rabenhorst BM, Morello R. Osteogenesis imperfecta: an update on clinical features and therapies. Eur J Endocrinol. 2020;183:R95-106. [Crossref]
- Tan LO, Lim SY, Vasanwala RF. Primary osteoporosis in children. BMJ Case Rep. 2017;2017:bcr2017220700. [Crossref]
- Rauch F, Travers R, Norman ME, Taylor A, Parfitt AM, Glorieux FH. Deficient bone formation in idiopathic juvenile osteoporosis: a histomorphometric study of cancellous iliac bone. J Bone Miner Res. 2000;15:957-63. [Crossref]
- Wang LT, Chen LR, Chen KH. Hormone-related and drug-induced osteoporosis: a cellular and molecular overview. Int J Mol Sci. 2023;24:5814. [Crossref]
- Sakka SD, Cheung MS. Management of primary and secondary osteoporosis in children. Ther Adv Musculoskelet Dis. 2020;12:1759720X20969262. [Crossref]
- Frost HM. Bone’s mechanostat: a 2003 update. Anat Rec A Discov Mol Cell Evol Biol. 2003;275:1081-101. [Crossref]
- Uziel Y, Zifman E, Hashkes PJ. Osteoporosis in children: pediatric and pediatric rheumatology perspective: a review. Pediatr Rheumatol Online J. 2009;7:16. [Crossref]
- von Scheven E, Corbin KJ, Stagi S, Cimaz R. Glucocorticoid-associated osteoporosis in chronic inflammatory diseases: epidemiology, mechanisms, diagnosis, and treatment. Curr Osteoporos Rep. 2014;12:289-99. [Crossref]
- Presedo A, Dabney KW, Miller F. Fractures in patients with cerebral palsy. J Pediatr Orthop. 2007;27:147-53. [Crossref]
- King WM, Ruttencutter R, Nagaraja HN, et al. Orthopedic outcomes of long-term daily corticosteroid treatment in Duchenne muscular dystrophy. Neurology. 2007;68:1607-13. [Crossref]
- Weinstein RS, Jilka RL, Parfitt AM, Manolagas SC. Inhibition of osteoblastogenesis and promotion of apoptosis of osteoblasts and osteocytes by glucocorticoids. Potential mechanisms of their deleterious effects on bone. J Clin Invest. 1998;102:274-82. [Crossref]
- Bertuna G, Famà P, Lo Nigro L, Russo-Mancuso G, Di Cataldo A. Marked osteoporosis and spontaneous vertebral fractures in children: don’t forget, it could be leukemia. Med Pediatr Oncol. 2003;41:450-1. [Crossref]
- Salim H, Ariawati K, Suryawan WB, Arimbawa M. Osteoporosis resulting from acute lymphoblastic leukemia in a 7-year-old boy: a case report. J Med Case Rep. 2014;8:168. [Crossref]
- Pepe J, Body JJ, Hadji P, et al. Osteoporosis in premenopausal women: a clinical narrative review by the ECTS and the IOF. J Clin Endocrinol Metab. 2020;105:dgaa306. [Crossref]
- Abraham A, Cohen A, Shane E. Premenopausal bone health: osteoporosis in premenopausal women. Clin Obstet Gynecol. 2013;56:722-9. [Crossref]
- Formosa MM, Christou MA, Mäkitie O. Bone fragility and osteoporosis in children and young adults. J Endocrinol Invest. 2024;47:285-98. [Crossref]
- Schini M, Vilaca T, Gossiel F, Salam S, Eastell R. Bone turnover markers: basic biology to clinical applications. Endocr Rev. 2023;44:417-73. [Crossref]
- Bishop N, Arundel P, Clark E, et al. Fracture prediction and the definition of osteoporosis in children and adolescents: the ISCD 2013 Pediatric Official Positions. J Clin Densitom. 2014;17:275-80. [Crossref]
- Ferrari S, Bianchi ML, Eisman JA, et al. Osteoporosis in young adults: pathophysiology, diagnosis, and management. Osteoporos Int. 2012;23:2735-48. [Crossref]
- Zemel BS, Leonard MB, Kelly A, et al. Height adjustment in assessing dual energy x-ray absorptiometry measurements of bone mass and density in children. J Clin Endocrinol Metab. 2010;95:1265-73. [Crossref]
- Lentle BC, Hammond I, Leslie WD, et al. The diagnosis of osteoporotic vertebral fractures redux. Clin Radiol. 2022;77:75-7. [Crossref]
- Crabtree NJ, Chapman S, Högler W, et al. Vertebral fractures assessment in children: evaluation of DXA imaging versus conventional spine radiography. Bone. 2017;97:168-74. [Crossref]
- Diacinti D, Pisani D, Cipriani C, et al. Vertebral fracture assessment (VFA) for monitoring vertebral reshaping in children and adolescents with osteogenesis imperfecta treated with intravenous neridronate. Bone. 2021;143:115608. [Crossref]
- van Dijk FS. Genetics of osteoporosis in children. Endocr Dev. 2015;28:196-209. [Crossref]
- Formosa MM, Bergen DJM, Gregson CL, et al. A roadmap to gene discoveries and novel therapies in monogenic low and high bone mass disorders. Front Endocrinol (Lausanne). 2021;12:709711. [Crossref]
- Muñoz-Garach A, García-Fontana B, Muñoz-Torres M. Nutrients and dietary patterns related to osteoporosis. Nutrients. 2020;12:1986. [Crossref]
- Ward LM, Ma J, Lang B, et al. Bone morbidity and recovery in children with acute lymphoblastic leukemia: results of a six-year prospective cohort study. J Bone Miner Res. 2018;33:1435-43. [Crossref]
- Birnkrant DJ, Bushby K, Bann CM, et al. Diagnosis and management of Duchenne muscular dystrophy, part 2: respiratory, cardiac, bone health, and orthopaedic management. Lancet Neurol. 2018;17:347-61. [Crossref]
- Ward LM, Konji VN, Ma J. The management of osteoporosis in children. Osteoporos Int. 2016;27:2147-79. [Crossref]
- Ward LM. A practical guide to the diagnosis and management of osteoporosis in childhood and adolescence. Front Endocrinol (Lausanne). 2024;14:1266986. [Crossref]
- Glorieux FH, Bishop NJ, Plotkin H, Chabot G, Lanoue G, Travers R. Cyclic administration of pamidronate in children with severe osteogenesis imperfecta. N Engl J Med. 1998;339:947-52. [Crossref]
- Trejo P, Rauch F. Osteogenesis imperfecta in children and adolescents-new developments in diagnosis and treatment. Osteoporos Int. 2016;27:3427-37. [Crossref]
- Galindo-Zavala R, Bou-Torrent R, Magallares-López B, et al. Expert panel consensus recommendations for diagnosis and treatment of secondary osteoporosis in children. Pediatr Rheumatol Online J. 2020;18:20. [Crossref]
- Simm PJ, Biggin A, Zacharin MR, et al. Consensus guidelines on the use of bisphosphonate therapy in children and adolescents. J Paediatr Child Health. 2018;54:223-33. [Crossref]
- Barros ER, Saraiva GL, de Oliveira TP, Lazaretti-Castro M. Safety and efficacy of a 1-year treatment with zoledronic acid compared with pamidronate in children with osteogenesis imperfecta. J Pediatr Endocrinol Metab. 2012;25:485-91. [Crossref]
- Kızılcan Çetin S, Şıklar Z, Aycan Z, et al. Clinical characteristics and treatment outcomes of children with primary osteoporosis. Turk Arch Pediatr. 2023;58:314-21. [Crossref]
- Nasomyont N, Hornung LN, Gordon CM, Wasserman H. Outcomes following intravenous bisphosphonate infusion in pediatric patients: a 7-year retrospective chart review. Bone. 2019;121:60-7. [Crossref]
- George S, Weber DR, Kaplan P, Hummel K, Monk HM, Levine MA. Short-term safety of zoledronic acid in young patients with bone disorders: an extensive institutional experience. J Clin Endocrinol Metab. 2015;100:4163-71. [Crossref]
- Lasky S, Moshal T, Shakoori P, et al. The risk of medication-related osteonecrosis of the jaw in children: guidance for antiresorptive use in pediatric patients. J Oral Maxillofac Surg. 2024;82:1285-94. [Crossref]
- Vasanwala RF, Sanghrajka A, Bishop NJ, Högler W. Recurrent proximal femur fractures in a teenager with osteogenesis imperfecta on continuous bisphosphonate therapy: are we overtreating? J Bone Miner Res. 2016;31:1449-54. [Crossref]
- Munns CF, Rauch F, Zeitlin L, Fassier F, Glorieux FH. Delayed osteotomy but not fracture healing in pediatric osteogenesis imperfecta patients receiving pamidronate. J Bone Miner Res. 2004;19:1779-86. [Crossref]
- Vyskocil V, Pikner R, Kutílek S. Effect of alendronate therapy in children with osteogenesis imperfecta. Joint Bone Spine. 2005;72:416-23. [Crossref]
- MacDonald P, Cranston A, Virdee M, Farncombe T, Athale U, Barr RD. Safety and efficacy of alendronate to treat osteopenia in children during therapy for acute lymphoblastic leukemia: a retrospective cohort study of sequential outcomes. J Pediatr Hematol Oncol. 2023;45:200-6. [Crossref]
- Bishop N, Adami S, Ahmed SF, et al. Risedronate in children with osteogenesis imperfecta: a randomised, double-blind, placebo-controlled trial. Lancet. 2013;382:1424-32. [Crossref]
- Shapiro JR, Thompson CB, Wu Y, Nunes M, Gillen C. Bone mineral density and fracture rate in response to intravenous and oral bisphosphonates in adult osteogenesis imperfecta. Calcif Tissue Int. 2010;87:120-9. [Crossref]
- Rauch F, Cornibert S, Cheung M, Glorieux FH. Long-bone changes after pamidronate discontinuation in children and adolescents with osteogenesis imperfecta. Bone. 2007;40:821-7. [Crossref]
- Biggin A, Zheng L, Briody JN, Coorey CP, Munns CF. The long-term effects of switching from active intravenous bisphosphonate treatment to low-dose maintenance therapy in children with osteogenesis imperfecta. Horm Res Paediatr. 2015;83:183-9. [Crossref]
- Boyce AM. Denosumab: an emerging therapy in pediatric bone disorders. Curr Osteoporos Rep. 2017;15:283-92. [Crossref]
- Vanderniet JA, Szymczuk V, Högler W, et al. Management of RANKL-mediated disorders with denosumab in children and adolescents: a global expert guidance document. J Clin Endocrinol Metab. 2024;109:1371-82. [Crossref]
- Liu J, Lin X, Sun L, et al. Safety and efficacy of denosumab in children with osteogenesis imperfecta-the first prospective comparative study. J Clin Endocrinol Metab. 2024;109:1827-36. [Crossref]
- Seale E, Molina MO, Carsen S, et al. Mitigating the denosumab-induced rebound phenomenon with alternating short- and long-acting anti-resorptive therapy in a young boy with severe OI type VI. Calcif Tissue Int. 2023;112:613-20. [Crossref]
- Lee SLK, Lim A, Munns C, Simm PJ, Zacharin M. Effect of testosterone treatment for delayed puberty in duchenne muscular dystrophy. Horm Res Paediatr. 2020;93:108-18. [Crossref]
- Black DM, Rosen CJ. Clinical practice. Postmenopausal osteoporosis. N Engl J Med. 2016;374:254-62. [Crossref]
- Ward LM, Rauch F. Anabolic Therapy for the treatment of osteoporosis in childhood. Curr Osteoporos Rep. 2018;16:269-76. [Crossref]
- Högler W, Shaw N. Childhood growth hormone deficiency, bone density, structures and fractures: scrutinizing the evidence. Clin Endocrinol (Oxf). 2010;72:281-9. [Crossref]
- Marini JC, Hopkins E, Glorieux FH, et al. Positive linear growth and bone responses to growth hormone treatment in children with types III and IV osteogenesis imperfecta: high predictive value of the carboxyterminal propeptide of type I procollagen. J Bone Miner Res. 2003;18:237-43. [Crossref]
- Ominsky MS, Vlasseros F, Jolette J, et al. Two doses of sclerostin antibody in cynomolgus monkeys increases bone formation, bone mineral density, and bone strength. J Bone Miner Res. 2010;25:948-59. [Crossref]
- Aditya S, Rattan A. Sclerostin inhibition: a novel target for the treatment of postmenopausal osteoporosis. J Midlife Health. 2021;12:267-75. [Crossref]
Copyright and license
Copyright © 2024 The author(s). This is an open-access article published by Aydın Pediatric Society under the terms of the Creative Commons Attribution License (CC BY) which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.