Abstract
Guillain-Barré syndrome (GBS) is an acute immune-mediated demyelinating disease. Early recognition of this disease is crucial as it can progress to life-threatening conditions such as respiratory failure or autonomic dysfunction. Typical clinical signs of GBS include progressive weakness of the extremities, bulbar muscles, and ophthalmoplegia. In pediatric cases, acute bladder dysfunction is more suggestive of acute myelopathy. In this study, we aimed to raise awareness about this rare but serious condition by presenting one of the youngest pediatric GBS cases in the literature, who presented with acute urinary retention as the first finding and was successfully treated with intravenous immunoglobulin.
Keywords: acute urinary retention, Guillain-Barré syndrome, pediatric
INTRODUCTION
Acute urinary retention (AUR) is rarely observed in otherwise healthy children.1 Common causes include urinary tract infections, severe constipation, and urinary stones. However, more serious conditions such as acute flaccid paralysis should also be considered due to their potentially severe consequences.2,3
This report aims to raise awareness about Guillain-Barré syndrome, a rare cause of AUR, and to emphasize the importance of a detailed neurological examination in a previously healthy female child presenting with AUR.
CASE PRESENTATION
A six-year-old girl was admitted to the pediatric emergency department and evaluated by a pediatric surgeon for severe abdominal pain and acute urinary retention, which had developed within 12 hours. She was admitted to the pediatric ward. The patient had a history of an upper respiratory tract infection approximately two weeks prior to the onset of symptoms. On physical examination, the patient exhibited suprapubic fullness and discomfort, consistent with bladder distention. A Foley catheter was inserted, confirming acute urinary retention by draining a large volume of urine.
The patient was referred to the pediatric neurology department. On initial neurological examination, the absence of deep tendon reflexes in all extremities was noted. The patient’s gag reflex was preserved, and there were no signs of ophthalmoplegia, ataxia, or other cranial nerve abnormalities. However, on the second day of hospitalization, she began to exhibit new-onset bilateral leg pain and decreased sensory perception in the lower extremities, and impaired ability to walk on tiptoes. Additionally, muscle strength was decreased (4/5) in all extremities. Moreover, no other signs or symptoms of autonomic dysfunction were observed during clinical follow-up. Intermittent urinary catheterization was administered four times per day throughout the duration of urinary retention.
An electromyography (EMG) study was conducted due to the emerging neurological symptoms, including weakness during tiptoe walking and complaints of constipation. The EMG revealed F-responses were absent and findings compatible with acute inflammatory demyelinating polyradiculoneuropathy (AIDP), the most common variant of Guillain-Barré Syndrome.
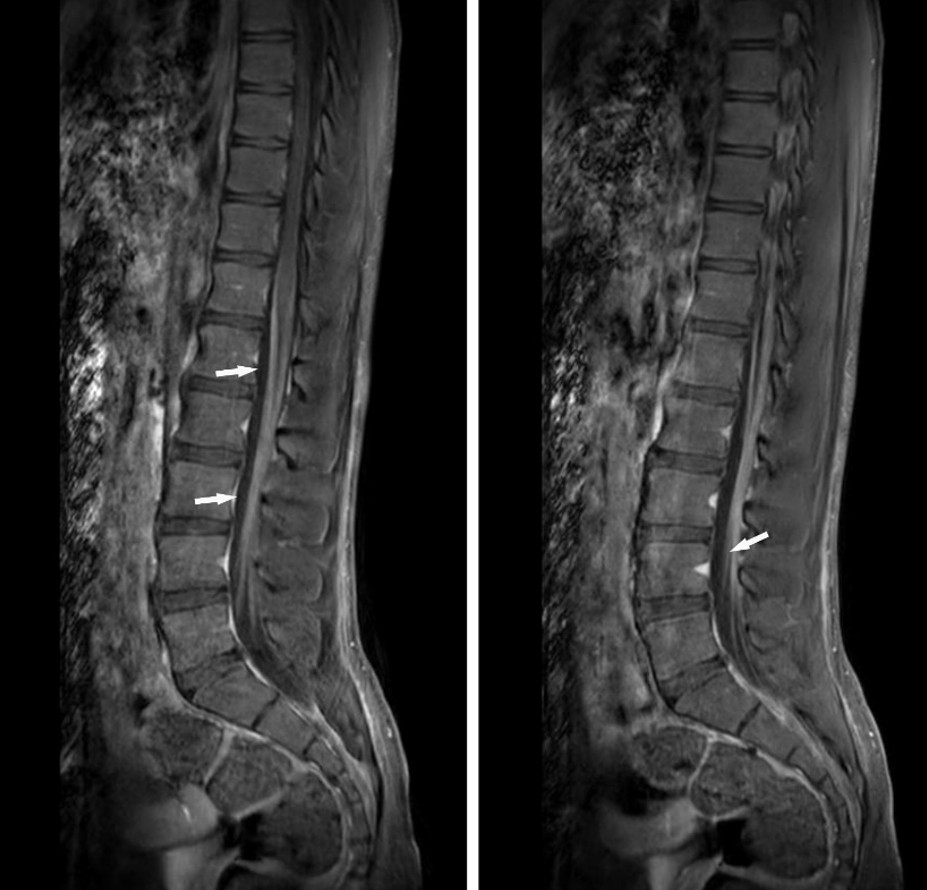
Spinal MRI with contrast revealed pathological enhancement of the cauda equina nerve roots in the sagittal sequence, further supporting the diagnosis (Figure 1). Cerebrospinal fluid (CSF) analysis via lumbar puncture demonstrated albuminocytologic dissociation: elevated protein level (57 mg/dL; reference range: 15–45 mg/dL) with no white blood cells. CSF glucose was within normal limits. No oligoclonal bands were detected, and polymerase chain reaction (PCR) testing was negative for herpes simplex virus, varicella zoster virus, and enterovirus. Serologic evaluations for coeliac disease, paraneoplastic syndromes, and anti-ganglioside antibodies were also negative.
The patient was diagnosed with Guillain-Barré Syndrome presenting as the AIDP variant and treated with intravenous immunoglobulin (IVIG) (2 gr/kg total dose, 0,4 gr/kg for five days) and supportive physical therapy. Marked clinical improvement was observed by the sixth day of treatment. At the 30-day follow-up, the patient’s neurological examination was completely normal, and she reported no residual symptoms.
DISCUSSION
Guillain-Barré syndrome is a disease that typically develops after an infection, which causes acute weakness and occurs at an incidence of 1.2-2.3 per 100,000 people annually. GBS typically presents with rapidly progressing weakness (within a few days), often associated with pain, sensory disturbances, and paresthesia symmetrically affecting the extremities. Involvement of the respiratory muscles can lead to respiratory failure and mortality. Approximately 2/3 of patients develop autonomic dysfunction.1,2,4
Mortality, which is the most critical complication in the first month of Guillain-Barré syndrome, has a significant rate. However, this is usually the case in initially misdiagnosed cases, as the initial symptoms are often nonspecific and many clinical variants can occur. Therefore, suspicion is crucial for early diagnosis and accelerating treatment. AUR is quite rare among pediatric GBS cases.1,4,5 Our case is one of the youngest reported patients presenting with AUR.
Involvement of non-limb muscles is rather an unusual presentation of GBS, and acute urinary retention has been reported in as low as 10% of cases.4 This is thought to be caused by a combination of hypo- and hyperactivity in both parasympathetic and sympathetic innervation of the bladder and urethra. AUR in GBS is primarily attributed to autonomic nervous system involvement, particularly affecting the innervation of the bladder and urethral sphincters. Dysregulation of sympathetic and parasympathetic pathways may lead to detrusor underactivity or sphincter dyssynergia, resulting in impaired bladder emptying. Several studies have shown that autonomic dysfunction, including cardiovascular and urogenital disturbances, occurs in up to two-thirds of GBS patients, even in the early stages and in mild forms of GBS.1,2,6 The fact that our patient presented with AUR in the early stage, there was no other autonomic system involvement, and weakness developed later shows that pediatric cases can present with different clinical pictures, similar to older cases.
There are many variants of GBS. Acute Inflammatory Demyelinating Polyneuropathy (AIDP) is the most common variant of GBS cases. In the AIDP form, peripheral nerve remyelination occurs relatively faster within weeks compared to other forms, leading to a better prognosis.5,6 Our patient suffered from the AIDP variant of GBS, which strongly supports her good recovery.
In conclusion, GBS is an acute immune-mediated demyelinating disease. Early recognition of this disease is crucial as it can progress to life-threatening conditions such as respiratory failure or autonomic dysfunction. Typical clinical manifestations of GBS include progressive weakness of the limbs, bulbar, facial muscles, and ophthalmoplegia. We report an early school-age pediatric case of GBS presenting with acute urinary retention, which was successfully treated with IVIG.
Ethical approval
Written informed consent was obtained from the participants.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Yuki N, Hartung HP. Guillain-Barré syndrome. N Engl J Med. 2012;366:2294-304. https://doi.org/10.1056/NEJMra1114525
- Gubbiotti M, Mahfouz W, Asimakopoulos AD, et al. COVID-19- associated Guillain-Barrè Syndrome and Urinary Dysfunction: a case report. Continence reports. 2022;4:100017. https://doi.org/10.1016/j.contre.2022.100017
- Evans OB, Vedanarayanan V. Guillain-Barré syndrome. Pediatr Rev. 1997;18:10-6. https://doi.org/10.1542/pir.18-1-10
- Labovitz AE, Mangurten HH. Guillain-Barré syndrome presenting with urinary retention and hypertension. Clin Pediatr (Phila). 2004;43:659-61. https://doi.org/10.1177/000992280404300713
- Khoo CS, Ali AH, Remli R, Tan HJ. A case of Guillain-Barré syndrome (GBS) presenting with acute urinary retention and T6 sensory level. Clin Med (Lond). 2018;18:308-10. https://doi.org/10.7861/clinmedicine.18-4-308
- Maleknasr SM, Crawley D, James FA. Inflammatory polyneuropathy presenting as acute urinary retention. BJU Int. 2011.
Copyright and license
Copyright © 2025 The author(s). This is an open-access article published by Aydın Pediatric Society under the terms of the Creative Commons Attribution License (CC BY) which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.