Abstract
Bronchopulmonary vascular malformations constitute a broad spectrum of developmental disorders in which a part of the lung is perfused exclusively from the systemic arterial tree with or without tracheobronchial communication. Pseudosequestration is a rare congenital pulmonary anomaly involving a lung segment with abnormal systemic arterial supply but a preserved connection to the bronchial tree. We present the case of a 5-month-old male referred for evaluation of a cardiac murmur. Initial investigations, including laboratory tests and chest X-ray, revealed ground-glass opacities in the left lung, prompting further imaging. Thoracic computed tomography (CT) and CT angiography demonstrated an aberrant systemic artery originating from the descending aorta and supplying the left lower lobe. Digital subtraction angiography (DSA) was subsequently performed to rule out vascular malformations and confirmed the diagnosis of pseudosequestration. Endovascular treatment was successfully completed with coil embolization and occlusion of the aberrant vessel using an Amplatzer Vascular Plug. The patient remained asymptomatic during a 20-month follow-up period. The case underscores the critical role of early recognition and noninvasive imaging in managing rare congenital pulmonary vascular anomalies.
Keywords: child, pseudosequestration, pulmonary
INTRODUCTION
Normal bronchial connection while receiving anomalous systemic arterial nutrition is an extremely rare pathology and may be difficult to recognize in relatively uncomplicated periods of life. Symptoms may manifest later in life as a consequence of left-sided volume overload resulting from a left-to-left shunt due to abnormal and large aberrant arterial feeding. Symptomatic patients typically present with hemoptysis, exertional dyspnea, pulmonary hypertension, and congestive cardiac failure.1 Despite its aberrant arterial supply, the defining feature distinguishing pseudosequestration from pulmonary sequestration is its preserved connection to the bronchial tree. No abnormal venous connections or distinct nidus formations, such as those observed in arteriovenous malformations, are present.
Thoracic computed tomography (CT) and CT angiography are the most accessible, noninvasive, and essential diagnostic tools for identifying normal lung parenchyma and isolated abnormal arterial relationships associated with this condition.2 In cases of pseudosequestration, the basal segments of the left lung are most frequently affected, with no radiographic abnormalities detected in the involved lung parenchyma.3 We present a case of pseudosequestration involving an anomalous systemic arterial supply to a morphologically normal basal segment of the left lower lobe. This case stands out due to its incidental diagnosis in an asymptomatic infant and the successful endovascular treatment that followed
CASE REPORT
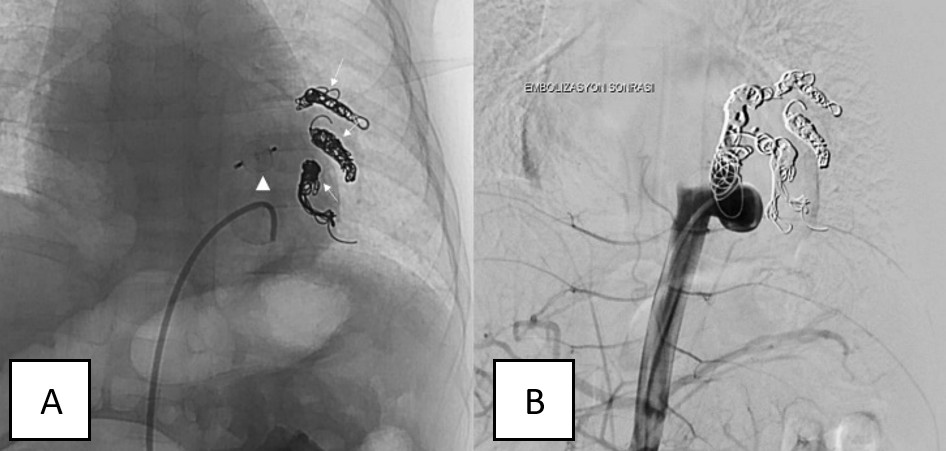
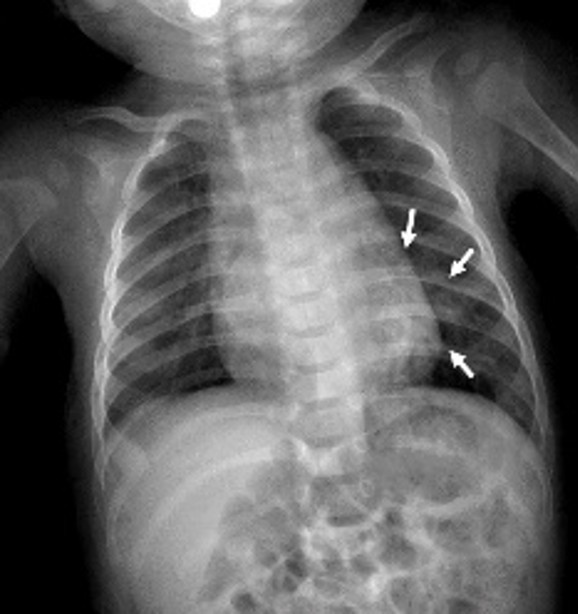
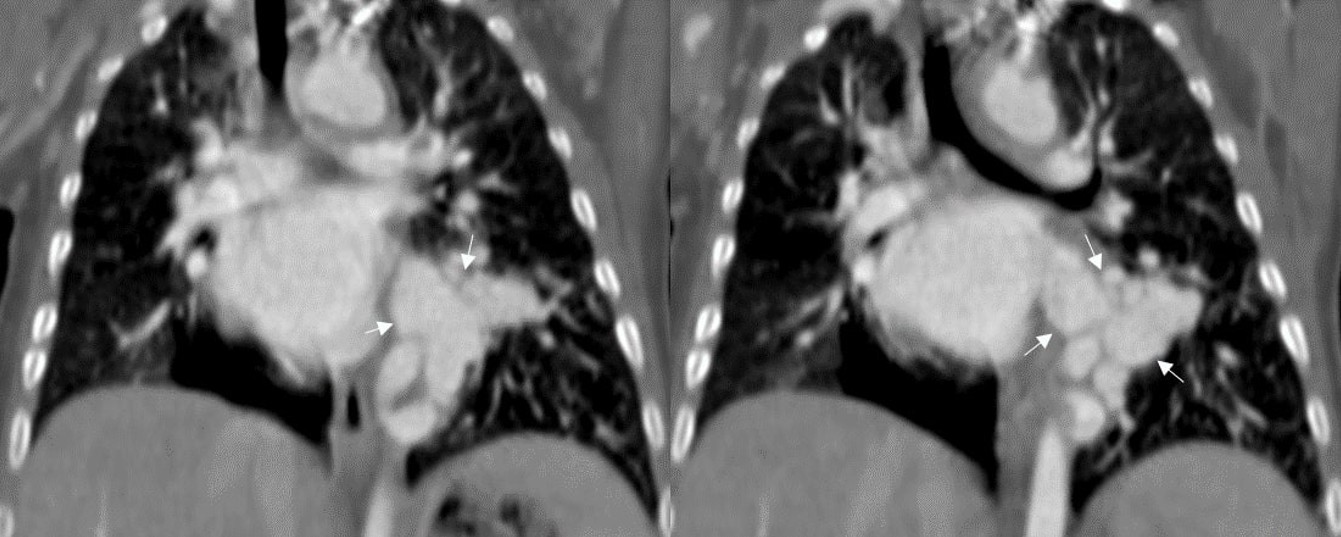
A 5-month-old infant was referred to our hospital after a suspected cardiac murmur was detected during a routine health check-up. Born via cesarean section at 39 weeks, the patient had no history of neonatal hospitalization, respiratory distress, or episodes of infection or bronchiolitis. Routine laboratory tests, including a complete blood count and assessments of kidney and liver function, were all normal. Chest X-ray revealed ground-glass opacities in the left upper and middle lung zones and opacification in the left lower zone (Figure 1). Thoracic CT and CT angiography were performed for further evaluation, with CT angiography demonstrating an aberrant vessel originating from the supradiaphragmatic descending aorta (Figure 2). This large systemic artery had three branches supplying the left lower lobe. Venous drainage from the affected lung parenchyma occurred via a dilated, tortuous left inferior pulmonary vein into the left atrium (Figure 3). No parenchymal abnormalities were observed, and the left lower lobe bronchus and its segmental branches appeared normal. These findings supported a diagnosis of pseudosequestration, as the affected lobe maintained a connection with the bronchial tree, differentiating it from true sequestration.
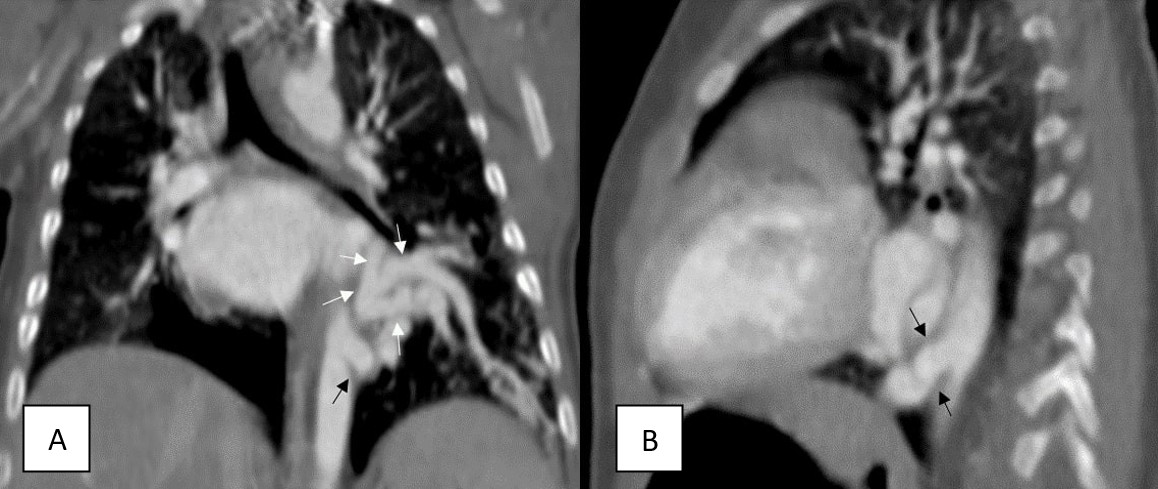
To confirm the diagnosis and exclude arteriovenous malformation, digital subtraction angiography (DSA) was performed (Figure 4). The DSA findings were consistent with the CT findings, and the aberrant branches were embolized with coils. The primary aberrant systemic artery, measuring 6.6 mm in its proximal segment, was occluded with an Amplatzer Vascular Plug, effectively terminating the aberrant arterial supply (Figure 5). No complications were observed during a 7-month follow-up period.
DISCUSSION
Pulmonary sequestration is a bronchopulmonary foregut malformation (BPFM) in which segmental lung tissue forms without connection to the bronchial tree or pulmonary arteries. Sequestration is classified as interlobar or extralobar based on the pleural relationship of the aberrant segment.4 In cases of pseudosequestration, the lung maintains normal communication with the tracheobronchial tree. It is most frequently observed in the left lower lobe, with its blood supply typically originating from an artery branching off the descending thoracic aorta. There is no abnormal venous drainage in this anomaly. This rare congenital anomaly is usually detected incidentally in infants and typically involves the lower lobes, where the blood supply is from an artery branching from the descending thoracic aorta.5,6 Yamanaka et al. reviewed 12 cases of systemic arterialization of lung segments, of which six patients were under six years of age. The predominant characteristics included male sex, left-sided involvement, and the descending thoracic aorta as the origin of the aberrant artery. In all cases, a single aberrant artery supplied the basal segments of the lower lobe of the lung. 7 In our patient, involvement of the left lower lobe and an aberrant arterial structure originating from the thoracic aorta were identified.
The development of this malformation is explained by the arrest of pulmonary artery growth during the development of the bronchial tree, resulting in an absence of pulmonary blood supply. Pseudosequestration may be congenital or may arise as a consequence of acquired conditions such as bronchiectasis, pulmonary tuberculosis, pulmonary infections, pulmonary thromboembolism, or chronic obstructive pulmonary disease. In affected patients, symptoms may also be attributable to the underlying disease.8 Primary patients may present with symptoms such as murmur, hemoptysis, exertional dyspnea, pulmonary hypertension, and congestive cardiac failure.1 Given the severity of these complications, early diagnosis and timely intervention are of critical importance. In this case, the only clinical finding was an incidentally detected cardiac murmur.
CT imaging is the preferred noninvasive modality for diagnosing pseudosequestration, providing essential information on the origin of the aberrant artery, its vascular supply, and native pulmonary artery anatomy.9 Additionally, CT enables the exclusion of other vascular malformations and confirms normal bronchial branching. Dual blood supply, originating from both the systemic and pulmonary arteries, has been reported in certain patients.8 CT angiography with 3D volumetric imaging and multiplanar reformations is invaluable for treatment planning and determining dual pathology.
As discussed by Yamanaka et al.,7 surgical resection, including lobectomy or segmentectomy, was often the primary approach in treating complicated cases. Endovascular treatments, such as coil embolization of the aberrant artery, present viable and less invasive alternatives. Singh et al.1 successfully treated an aberrant arterial structure originating from the thoracic aorta in the left lower lobe using coil embolization.
In this case, endovascular embolization was chosen over surgery for its minimally invasive approach, lower perioperative risk, and lung preservation. It successfully occluded the aberrant artery while maintaining normal bronchial and venous drainage. At 20 months of follow-up, the treated lung segment remains viable, with no signs of ischemia, fibrosis, or recurrent shunting, supporting the efficacy of this approach.
Pseudosequestration represents a rare congenital pulmonary anomaly involving a lung segment with aberrant arterial supply but a normal bronchial structure. Thoracic CT and CT angiography serve as crucial noninvasive diagnostic tools. Early diagnosis is essential to detect vascular abnormalities in otherwise normal lung parenchyma, as delayed detection can lead to complications such as pulmonary hypertension and heart failure. This case highlights the critical need to differentiate pseudosequestration from true sequestration due to their disparate management approaches.
Ethical approval
Written informed consent was obtained from the participants.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Singh AS, Subbain SK, Subramanian KG, et al. Pseudosequestration of the left lung. Tex Heart Inst J. 2007;34:195-8.
- Gormez A, Ozcan HN, Oguz B, et al. Rare presentation of pseudosequestration in childhood: CT and CT angiography findings. Clin Respir J. 2017;11:113-6. https://doi.org/10.1111/crj.12295
- Tao CW, Chen CH, Yuen KH, Huang MH, Li WY, Perng RP. Anomalous systemic arterial supply to normal basilar segments of the lower lobe of the left lung. Chest. 1992;102:1583-5. https://doi.org/10.1378/chest.102.5.1583
- Pryce DM. Lower accessory pulmonary artery with intralobar sequestration of lung; a report of seven cases. J Pathol Bacteriol. 1946;58:457-67.
- Erik N, Başlılar Ş, Kaya S, Şaylan B. Bronchopulmonary ‘pseudo’ sequestration. Respir Case Rep. 2019;8:119-22. https://doi.org/10.5505/respircase.2019.33603
- Akçam Tİ, Ergönül AG, Turhan K. A very rare cause of recurrent hemoptysis in a young male patient: pseudosequestration. Turk Gogus Kalp Damar Cerrahisi Derg. 2018;26:161-2. https://doi.org/10.5606/tgkdc.dergisi.2018.14538
- Yamanaka A, Hirai T, Fujimoto T, Hase M, Noguchi M, Konishi F. Anomalous systemic arterial supply to normal basal segments of the left lower lobe. Ann Thorac Surg. 1999;68:332-8. https://doi.org/10.1016/s0003-4975(99)00533-0
- Baek WK, Cho J, Kim JT, et al. Systemic arterial supply to normal basal segments of the left lower lobe along with the pulmonary artery: is lung resection warranted? J Thorac Cardiovasc Surg. 2006;131:742-3. https://doi.org/10.1016/j.jtcvs.2005.10.053
- Ko SF, Ng SH, Lee TY, et al. Anomalous systemic arterialization to normal basal segments of the left lower lobe: helical CT and CTA findings. J Comput Assist Tomogr. 2000;24:971-6. https://doi.org/10.1097/00004728-200011000-00026
Copyright and license
Copyright © 2025 The author(s). This is an open-access article published by Aydın Pediatric Society under the terms of the Creative Commons Attribution License (CC BY) which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.