Abstract
Objective: To evaluate the effect of pre-void and post-void bladder volume on the anteroposterior (AP) diameter of the renal pelvis in asymptomatic pediatric hydronephrosis and to determine its influence on ultrasonographic measurement variability.
Method: A retrospective analysis was conducted on 113 children aged 4–9 years who were referred for renal ultrasonography (US) between 2019 and 2023. Patients were excluded if they had end-stage renal disease, congenital anomalies of the kidney and urinary tract, polycystic kidney disease, bilateral hydronephrosis, prior renal surgery, suboptimal image quality, or pathological findings on additional diagnostic tests such as scintigraphy or voiding cystourethrography. Standardized protocols were used to measure the AP diameter of the renal pelvis and bladder volume in both pre-void and post-void states, utilizing the ellipsoid formula. Paired t-tests and Pearson’s correlation coefficient were applied for statistical analysis.
Results: The mean AP diameter of the renal pelvis significantly decreased from 7.43 ± 1.90 mm in the pre-void state to 5.62 ± 1.46 mm in the post-void state (p < 0.05). Similarly, bladder volume was markedly reduced from 183.6 ± 88.0 mL to 16.4 ± 14.9 mL (p < 0.05). Pearson’s correlation analysis revealed a strong positive correlation between pre-void bladder volume and the reduction in AP diameter (r = 0.65, p < 0.05), demonstrating the considerable effect of bladder volume on renal pelvic measurements.
Conclusion: Incorporating pre- and post-void measurements into routine renal ultrasound protocols may enhance diagnostic accuracy, reduce variability, and improve clinical decision-making in pediatric hydronephrosis evaluation.
Keywords: renal pelvis, hydronephrosis, ultrasonography, urinary bladder, volume, pediatrics, pre-void, post-void
INTRODUCTION
The widespread use of prenatal US has significantly increased the diagnosis of children with asymptomatic renal pelvic dilatation. Renal pelvic dilatation is a prognostic indicator in the initial diagnosis and follow-up of severe urological diseases. A critical measure in assessing hydronephrosis is the AP diameter of the renal pelvis, particularly how it changes over time in follow-up US examinations. For neonates, an AP diameter greater than 6 mm raises concerns about potential obstruction, while values exceeding 15 mm are strongly associated with severe uropathology, with sensitivity and specificity surpassing 90%.1-5 To address this, the Society for Fetal Urology’s grading system has become a widely accepted approach for classifying and managing such cases.6,7 Despite these advancements, measuring renal pelvis dimensions continues to face challenges, particularly due to factors such as the patient’s hydration level and bladder volume.
One of the most influential yet often overlooked factors in routine US is bladder volume. This variable can significantly alter the AP diameter of the renal pelvis, leading to variability in measurements. While some studies have examined the effects of hydration on renal pelvis dimensions, limited data exist regarding the impact of bladder volume on renal pelvis dimensions.8-10 Clarifying this relationship is essential to avoid diagnostic errors, which could otherwise result in unnecessary invasive tests or delays in treatment.
In line with our hypothesis that bladder volume has a significant impact on the renal pelvis diameter, we propose that bladder volume should be incorporated into the routine renal US evaluation protocol. We believe that this quantitative parameter could enhance diagnostic accuracy, minimize confounding variables, and reduce misleading results, thereby optimizing patient management. In this context, this study aims to investigate the effect of pre- and post-void bladder volume on the AP diameter of the renal pelvis in children under clinical and radiological follow-up for asymptomatic hydronephrosis.
MATERIAL AND METHOD
Study population
This study was approved by the local ethics committee (approval date: 24.10.2024; approval no: 632227). Pediatric patients aged 4–9 years who were under clinical follow-up for hydronephrosis and referred to the radiology department for ultrasonographic evaluation between January 2019 and January 2023 were retrospectively assessed. Radiological images of the patients were retrieved and reviewed from the picture archiving and communication system, while clinical data were obtained from the hospital information management system.
Only patients with clinically asymptomatic hydronephrosis and those under follow-up for renal pelvis AP diameter were included in the study. Patients with the following conditions were excluded from the study: (1) end-stage renal disease of any etiology, (2) congenital anomalies of the kidney and urinary tract (CAKUT), (3) polycystic kidney disease, and (4) history of prior renal surgery. Additionally, patients with suboptimal ultrasonographic image quality, measurement errors, missing data, or bilateral hydronephrosis were excluded to ensure a homogeneous study population. Patients with pathological findings on scintigraphy and/or voiding cystourethrography, as well as those with a renal pelvis AP diameter greater than 10 mm who had not undergone these diagnostic tests, were excluded. Nonetheless, a small subset of patients with a renal pelvis AP diameter greater than 10 mm but with normal findings on additional diagnostic tests were included. The images and clinical data of the patients were evaluated by two experienced radiologists. As a result, 113 patients met the inclusion criteria and were included in the final analysis.
Measurement technique
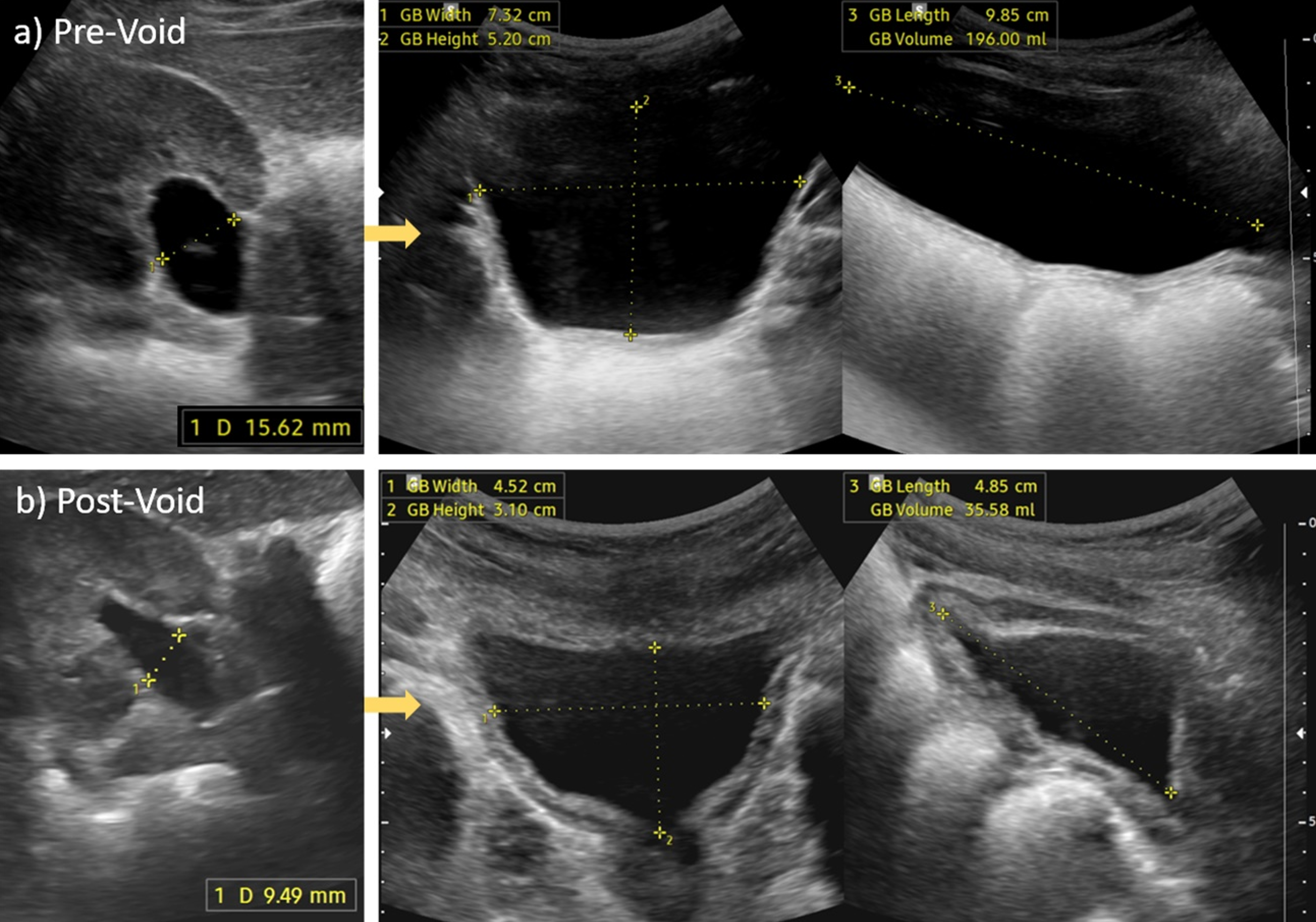
All US examinations were performed using RS-80A and HS-50 devices equipped with a convex array probe (CA1-7A, 1-7 MHz) (Samsung Medison Co., Ltd., Hongcheon, Korea). Renal US examinations were performed with the patient in the supine or lateral decubitus position, as deemed appropriate. The renal pelvis AP diameter was measured twice for each patient. The first measurement was taken before voiding, along with the calculation of bladder volume. The second measurement was performed immediately after voiding, and the residual bladder volume was also calculated.
The AP diameter of the renal pelvis was measured in the mid-renal transverse plane, along the longest axis where the renal hilum was visible, and at the level of the hilum.11 The measurement was taken from the inner edge to the inner edge of the pelvis, and the average of repeated measurements was recorded. The bladder volume was automatically calculated by the US device using the ellipsoid formula (L×W×D×0.523), where L represents the maximum length of the bladder, measured in the longitudinal plane from the bladder fundus to the internal urethral opening; W is the maximum width, measured in the transverse plane perpendicular to the midline at its midpoint; and D is the maximum depth, measured in the transverse plane along the midline from the anterior to posterior mucosal surface (Figure 1).12
Statistical analysis
All statistical analyses were performed using SPSS version 26.0 (IBM Corp., Armonk, NY, USA). Continuous variables were reported as mean ± standard deviation for normally distributed data. Categorical variables were presented as frequencies and percentages. The Shapiro–Wilk test was used to assess the normality of continuous variables. The primary analysis compared the renal pelvis AP diameter before and after voiding using the paired t-test, as the data followed a normal distribution. The association between pre-void bladder volume and the change in renal pelvis AP diameter was analyzed using Pearson’s correlation coefficient. A p-value <0.05 was considered statistically significant for all analyses.
RESULTS
Patient Demographics and Clinical Characteristics
A total of 113 patients were included in the study, with an age range of 4 to 9 years. The mean age of the patients was 6.3 ± 1.44 years, and the cohort comprised 59% males (n = 67) and 41% females (n = 46). Unilateral renal pelvis dilation was more common on the left side (n = 71, 63%) compared to the right side (n = 42, 37%).
Renal Pelvis and Bladder Volume Measurements
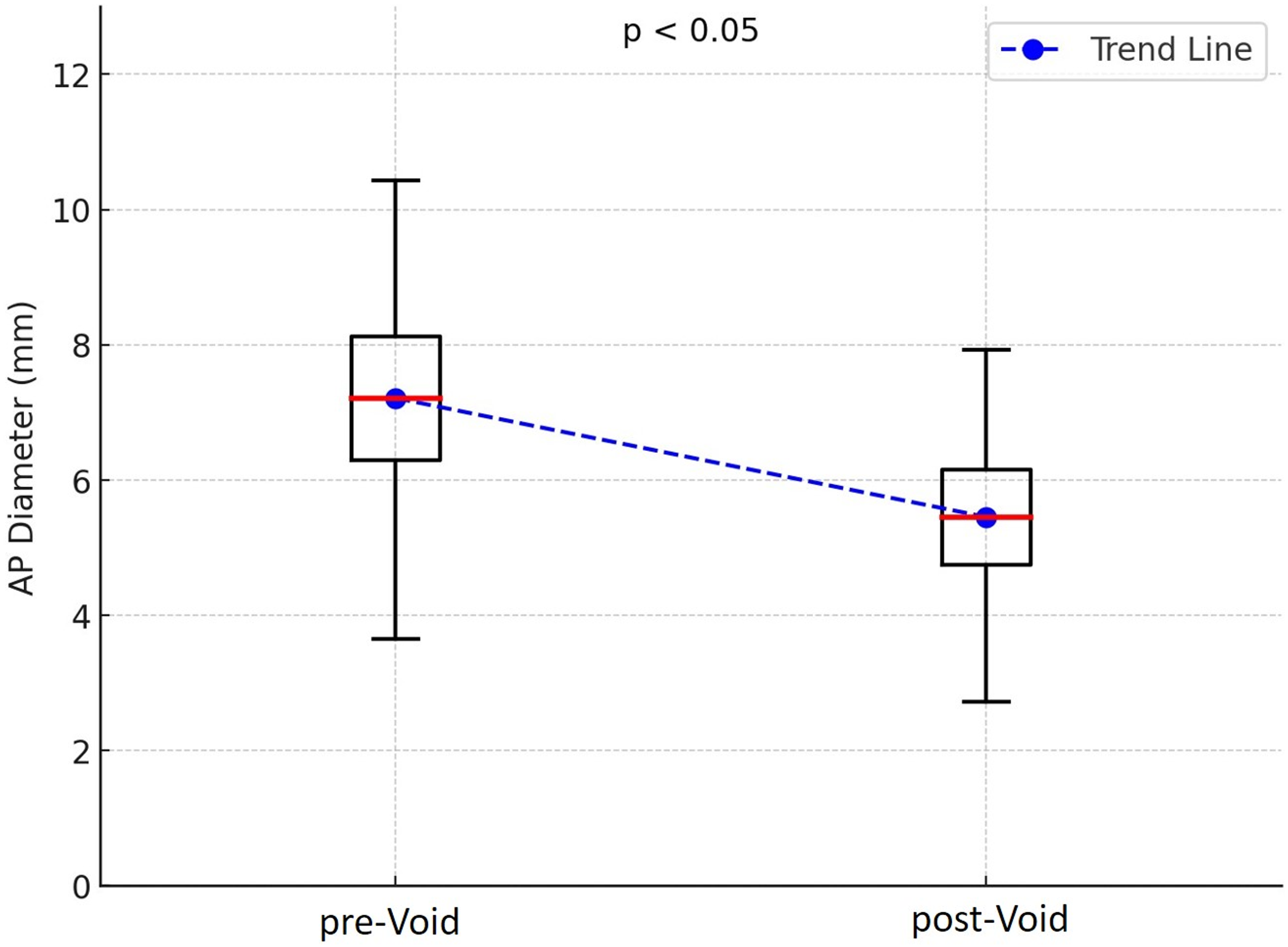
The mean AP diameter of the renal pelvis in the pre-void state was 7.43 ± 1.90 mm, which significantly decreased to 5.62 ± 1.46 mm in the post-void state (p < 0.05).
Similarly, the mean bladder volume decreased significantly from 183.6 ± 88.0 mL in the pre-void state to 16.4 ± 14.9 mL post-void (p < 0.05) (Table 1, Figure 2)
| *: Anterior-posterior. | |||
| Table 1. Pre-void and post-void measurements of renal pelvis diameter and bladder volume | |||
| Category |
|
|
|
| Renal pelvis AP* diameter (mm) |
|
|
|
| Bladder volume (mL) |
|
|
|
Correlation Between Bladder Volume and Renal Pelvis AP Diameter
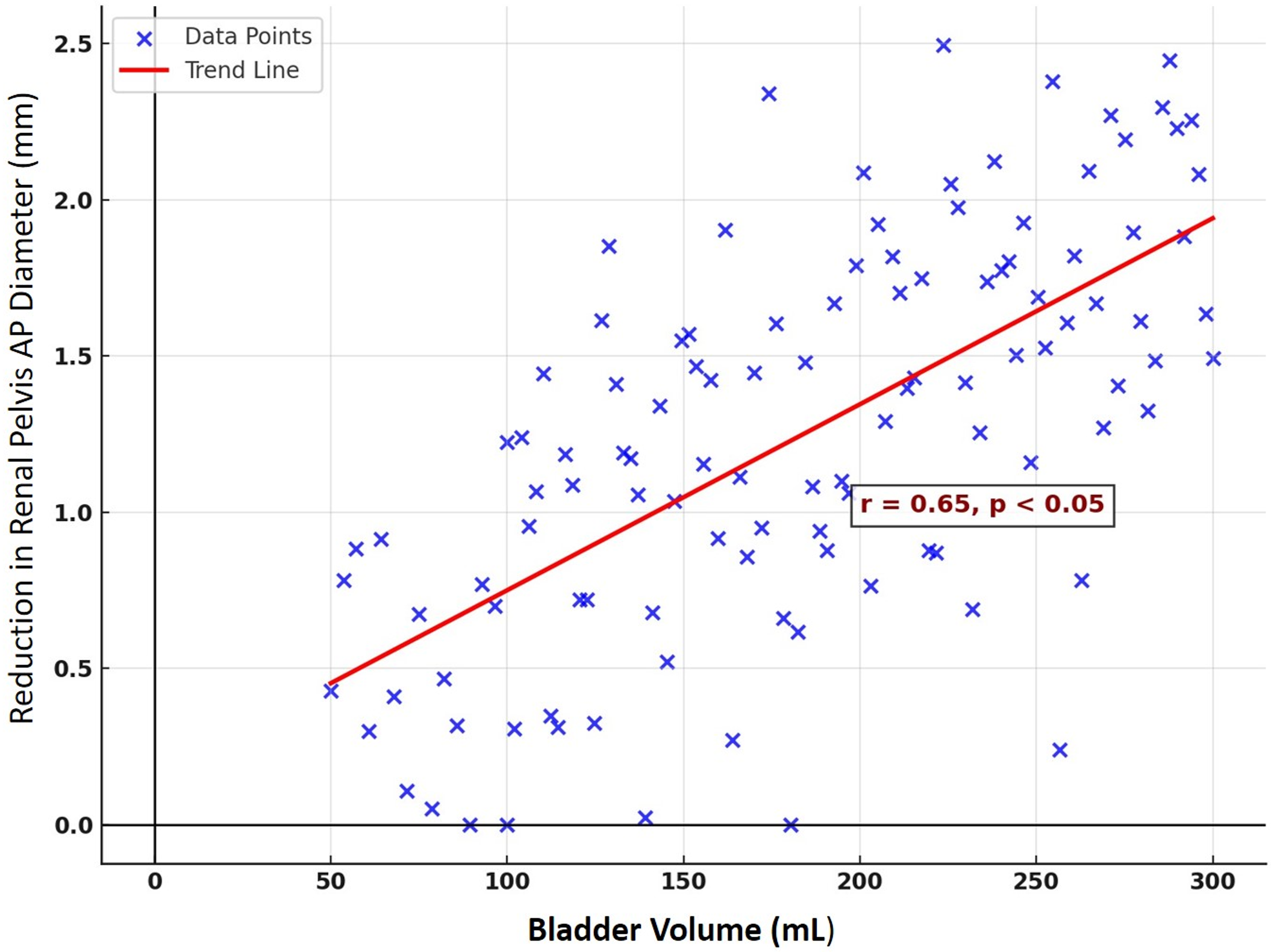
Pearson’s correlation analysis revealed a significant positive correlation between pre-void bladder volume and the reduction in post-void renal pelvis AP diameter (r = 0.65; p < 0.05). This finding suggests that higher bladder volumes were associated with greater decreases in renal pelvis AP diameter after voiding (Figure 3).
DISCUSSION
Ultrasonography serves as a fundamental tool in evaluating renal diseases in pediatric patients, owing to its non-invasive nature, safety, and widespread accessibility. This study highlights the significant impact of bladder volume on renal pelvis AP diameter measurements, offering a clearer perspective on the interpretation of such data.
Hydronephrosis is a common finding during prenatal US or those performed for various reasons, such as urinary tract infections. In such cases, invasive procedures are typically avoided if there is no significant dilatation of the collecting system, with follow-up commonly relying on the renal pelvis AP diameter. Several factors indirectly influence the AP diameter of the renal pelvis, one of which is hydration status. Studies have documented the effects of hydration on these measurements.13 Koff et al. reported that diuresis can cause dilatation of the collecting system, even in the absence of obstructive pathology, with this effect being more pronounced in non-obstructive conditions.14 In routine practice, renal US is performed under variable hydration conditions, with no clear recommendations regarding fluid intake or the timing of the examination. Consequently, it seems impractical to eliminate the influence of hydration on renal pelvis AP diameter.
Another variable affecting renal pelvis dilatation is bladder volume. Studies have explored the effect of bladder volume on renal pelvis measurements. For instance, Demir et al. demonstrated that bladder volume significantly influenced renal pelvis AP diameter in patients with vesicoureteral reflux, with a marked reduction observed after bladder emptying.15 Morin et al. emphasized that bladder volume can moderately dilate the ureter and pelvicalyceal system, recommending that renal US be performed with an empty bladder to prevent misinterpretation.16 Similarly, a comprehensive review of pediatric renal imaging suggested that empty bladder protocols should be implemented to enhance the reliability of US assessments.17 Leung et al. introduced the “hydronephrosis index,” calculated by dividing the renal pelvis AP diameter by the bladder volume to minimize the misleading effects of bladder volume on renal pelvis AP measurements.18 This correlation was validated in their study involving infant patients.19 Another study on neurogenic bladder dysfunction highlighted the impact of bladder volume on US measurements, underscoring the need for standardized protocols.20 Research on renal imaging principles also addressed the influence of bladder volume on renal pelvis AP measurements, advocating for emerging technologies to address these challenges.21 Additionally, the integration of urodynamics with the US has reinforced the importance of considering bladder volume in US protocols.22 Overall, the literature agrees on the significant influence of bladder volume on renal pelvis AP measurements. The quantitative findings of this study further support this consensus, underscoring the need for standardization.
The Society for Fetal Urology (SFU) and the European Society of Pediatric Radiology (ESPR) do not provide specific recommendations regarding the impact of bladder fullness on renal pelvis measurements in their current hydronephrosis assessment guidelines.2,23 Incorporating standardized pre- and post-void renal pelvis measurements into routine ultrasonographic protocols may reduce measurement inconsistencies and improve patient management strategies. Considering changes in bladder volume could enhance the precision of diagnostic decision-making and prevent the overestimation of hydronephrosis severity. Ultimately, this quantitative, data-driven approach may reduce the need for invasive tests in asymptomatic patients.
This study has several limitations. Its retrospective and single-center design may limit the generalizability of the findings, as patient demographics and sonographic techniques may vary across institutions. Additionally, ultrasonography is inherently operator-dependent, and although all images were reviewed by two experienced radiologists and suboptimal cases were excluded, some degree of interobserver variability may still be present. This study focused on asymptomatic hydronephrosis without a known pathology, but undiagnosed underlying conditions may have influenced the results. The lack of hydration status control constitutes a critical limitation. As hydration can physiologically alter the degree of renal pelvic dilatation, variability in fluid intake prior to imaging may have influenced the measurements. This factor was not standardized in our protocol and may affect the reproducibility and consistency of the results. Future studies should consider implementing controlled hydration protocols before ultrasound examinations to minimize measurement variability and enhance diagnostic reliability.
CONCLUSION
In conclusion, this study demonstrates that bladder volume has a significant and measurable impact on renal pelvis AP diameter, emphasizing its clinical relevance in pediatric renal US. Incorporating pre- and post-void measurements into standard US protocols may enhance diagnostic accuracy, minimize variability, and reduce the need for unnecessary invasive investigations in children with asymptomatic hydronephrosis. This approach may also promote consistency in longitudinal follow-up and support more reliable clinical decision-making.
Ethical approval
The study was approved by Aydın Adnan Menderes University Ethics Committee (date: 24.10.2024, number: 632227).
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Dias CS, Silva JMP, Pereira AK, et al. Diagnostic accuracy of renal pelvic dilatation for detecting surgically managed ureteropelvic junction obstruction. J Urol. 2013;190:661-6. https://doi.org/10.1016/j.juro.2013.02.014
- Nguyen HT, Herndon CDA, Cooper C, et al. The Society for Fetal Urology consensus statement on the evaluation and management of antenatal hydronephrosis. J Pediatr Urol. 2010;6:212-31. https://doi.org/10.1016/j.jpurol.2010.02.205
- Bouzada MCF, Oliveira EA, Pereira AK, et al. Diagnostic accuracy of postnatal renal pelvic diameter as a predictor of uropathy: a prospective study. Pediatr Radiol. 2004;34:798-804. https://doi.org/10.1007/s00247-004-1283-8
- Clautice-Engle T, Anderson NG, Allan RB, Abbott GD. Diagnosis of obstructive hydronephrosis in infants: comparison sonograms performed 6 days and 6 weeks after birth. AJR Am J Roentgenol. 1995;164:963-7. https://doi.org/10.2214/ajr.164.4.7726057
- Yiee J, Wilcox D. Management of fetal hydronephrosis. Pediatr Nephrol. 2008;23:347-53. https://doi.org/10.1007/s00467-007-0542-y
- Fernbach SK, Maizels M, Conway JJ. Ultrasound grading of hydronephrosis: introduction to the system used by the Society for Fetal Urology. Pediatr Radiol. 1993;23:478-80. https://doi.org/10.1007/BF02012459
- Maizels M, Mitchell B, Kass E, Fernbach SK, Conway JJ. Outcome of nonspecific hydronephrosis in the infant: a report from the Registry of the Society for Fetal Urology. J Urol. 1994;152:2324-7.
- Hasch E. Changes in renal pelvic size in children after fluid intake demonstrated by ultrasound. Ultrasound Med Biol. 1977;2:287-90. https://doi.org/10.1016/0301-5629(77)90028-x
- Peerboccus M, Damry N, Pather S, Devriendt A, Avni F. The impact of hydration on renal measurements and on cortical echogenicity in children. Pediatr Radiol. 2013;43:1557-65. https://doi.org/10.1007/s00247-013-2748-4
- Nicolau C, Vilana R, Del Amo M, et al. Accuracy of sonography with a hydration test in differentiating between excretory renal obstruction and renal sinus cysts. J Clin Ultrasound. 2002;30:532-6. https://doi.org/10.1002/jcu.10111
- Hodhod A, Eid H, Capolicchio JP, et al. How can we measure the renal pelvic anteroposterior diameter in postnatal isolated hydronephrosis? J Pediatr Urol. 2023;19:75-82. https://doi.org/10.1016/j.jpurol.2022.08.007
- Dicuio M, Pomara G, Menchini Fabris F, Ales V, Dahlstrand C, Morelli G. Measurements of urinary bladder volume: comparison of five ultrasound calculation methods in volunteers. Arch Ital Urol Androl. 2005;77:60-2.
- Alkan M, Tiryaki S, Özbek SS, Avanoğlu A, Ulman İ. The maximum anteroposterior diameter of renal pelvis changes by hydration in cases of ureteropelvic junction obstruction. Turkiye Klinikleri J Pediatr. 2013;22:105-9.
- Koff SA, Binkovitz L, Coley B, Jayanthi VR. Renal pelvis volume during diuresis in children with hydronephrosis: implications for diagnosing obstruction with diuretic renography. J Urol. 2005;174:303-7. https://doi.org/10.1097/01.ju.0000161217.47446.0b
- Demir S, Tokmak N, Cengiz N, Noyan A. Value of sonographic anterior-posterior renal pelvis measurements before and after voiding for predicting vesicoureteral reflux in children. J Clin Ultrasound. 2015;43:490-4. https://doi.org/10.1002/jcu.22260
- Morin ME, Baker DA. The influence of hydration and bladder distension on the sonographic diagnosis of hydronephrosis. J Clin Ultrasound. 1979;7:192-4. https://doi.org/10.1002/jcu.1870070306
- Viteri B, Calle-Toro JS, Furth S, Darge K, Hartung EA, Otero H. State-of-the-art renal imaging in children. Pediatrics. 2020;145:e20190829. https://doi.org/10.1542/peds.2019-0829
- Leung VYF, Chu WCW, Metreweli C. Hydronephrosis index: a better physiological reference in antenatal ultrasound for assessment of fetal hydronephrosis. J Pediatr. 2009;154:116-20. https://doi.org/10.1016/j.jpeds.2008.06.032
- Leung VYF, Rasalkar DD, Liu JX, Sreedhar B, Yeung CK, Chu WCW. Dynamic ultrasound study on urinary bladder in infants with antenatally detected fetal hydronephrosis. Pediatr Res. 2010;67:440-3. https://doi.org/10.1203/PDR.0b013e3181d22b91
- Bozbeyoğlu SG, Ersoy F, Canmemiş A, Khanmammadova N, Özel ŞK. Effect of bladder volume and compliance on ultrasonographic measurement of bladder wall thickness in children with neurogenic bladder dysfunction. J Pediatr Urol. 2024;20:243.e1-243.e9. https://doi.org/10.1016/j.jpurol.2023.11.015
- Leung VYF, Chu WCW, Yeung CK, et al. Nomograms of total renal volume, urinary bladder volume and bladder wall thickness index in 3,376 children with a normal urinary tract. Pediatr Radiol. 2007;37:181-8. https://doi.org/10.1007/s00247-006-0376-y
- Snow-Lisy DC, Nicholas J, Sturm R, et al. Integrated ultrasound with urodynamics illustrates effect of bladder volume on upper tract dilation: should we trust surveillance ultrasounds? Urology. 2022;159:203-209. https://doi.org/10.1016/j.urology.2021.08.007
- Vivier PH, Augdal TA, Avni FE, et al. Standardization of pediatric uroradiological terms: a multidisciplinary European glossary. Pediatr Radiol. 2018;48:291-303. https://doi.org/10.1007/s00247-017-4006-7
Copyright and license
Copyright © 2025 The author(s). This is an open-access article published by Aydın Pediatric Society under the terms of the Creative Commons Attribution License (CC BY) which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.














