Abstract
Background and Aim: Despite progress in HIV prevention and treatment in many regions, Eastern Europe and Central Asia continue to experience a rising epidemic, with a 20% increase in new HIV cases since 2010. Pediatric HIV remains a significant concern, with 13,000 children (0–14 years) living with HIV in Eastern Europe and Central Asia. Mother-to-child transmission (MTCT) rates in the region stand at 10%, far exceeding the global elimination targets of 2% (for non-breastfeeding mothers) and 5% (for breastfeeding mothers). However, country-specific, age-disaggregated data on pediatric HIV (prevalence, incidence, mortality, and ART coverage) remain scarce, hindering targeted interventions. This study aimed to assess the prevalence, incidence, and mortality of HIV among children under 5 years in Central Asia and evaluate health expenditures related to pediatric HIV treatment in the region.
Methods: This descriptive study includes prevalence, incidence of HIV, and all deaths of children under 5 years of age living with HIV, in different regions covered by Central Asia during the years 1990 to 2021. Information was collected from the mortality registration system. Financial data on HIV-related health spending for each country of interest were gathered through the Development Assistance to Health (DAH) database. The model framework was based on the Global Burden of Disease (GBD) protocol.
Results: There is a dramatic surge in HIV prevalence across Central Asia, from 4,776 cases in 1990 to over 1.5 million in 2019. Kazakhstan and Uzbekistan faced the most significant increases, while Georgia showed progress in reducing new infections, and Mongolia remained the least affected. Male children consistently had higher rates of HIV-related incidence and mortality. Notably, Uzbekistan experienced a rise in under-5 HIV-related mortality, from 10.06 per 100,000 in 1990 to 11.52 in 2019. Disparities in healthcare spending were evident, with Kazakhstan and Kyrgyzstan demonstrating more substantial investments, in contrast to lower per capita spending in Uzbekistan and Turkmenistan.
Conclusion: Overall, the Central Asian region is experiencing a surge in HIV cases among children under 5 years of age, which contrasts with global trends. This may be attributed to disparities in healthcare spending, access to care, prevention efforts, and the stigma associated with HIV in Central Asia.
Keywords: children living with HIV, human immunodeficiency virus (HIV), central Asian countries
INTRODUCTION
Acquired Immunodeficiency Syndrome (AIDS) is a severe, life-threatening condition caused by the Human Immunodeficiency Virus (HIV).1 HIV is the most common viral infection worldwide, according to the World Health Organization (WHO), and is increasing in high-risk groups, reaching more than 5 percent of the population.2 Currently, there is no vaccine for this disease, and prevention is considered the most important and effective method of combating the HIV epidemic in the world.3 The number of HIV-infected patients is declining in numerous African countries4, but in Eastern Europe and Central Asia, the number of new HIV cases acquired has increased by 20% since 2010. The region is not on track to meet the 2030 targets for ending AIDS. Moreover, Central Asian countries account for a significant portion of these cases, with four countries (Kazakhstan, the Russian Federation, Ukraine, and Uzbekistan) reporting 92% of all new registered HIV cases in the region, according to published case reports from 15 of 16 countries.5 This alarming trend extends to pediatric HIV, where significant challenges persist. While global efforts have reduced mother-to-child transmission (PMTCT) rates in many parts of the world, Eastern Europe and Central Asia still face hurdles. In Eastern Europe and Central Asia, an estimated 13,000 children aged 0-14 were living with HIV at the end of 2023, with 1,400 newly infected children in this age group in 2023.6
Currently, the main pattern of HIV in Central Asia includes transmission through injection drug users (IDUs). However, it seems that, like other parts of the world, these countries are rapidly moving towards a pattern of sexual transmission, which will also increase the perinatal risk of acquiring HIV.7 In developed countries, mother-to-child HIV transmission has decreased from 25% at the beginning of the epidemic to less than 2% in 2008.8,9 However, in Central Asia, mother-to-child transmission is still a significant concern. In 2023, the overall global mother-to-child transmission rate for Eastern Europe and Central Asia was 10%, which is still far from the 2% elimination threshold for non-breastfeeding countries and 5% for breastfeeding countries, indicating a critical need for intensified efforts in the region.10 While regional data exist, precise, country-specific, disaggregated data on pediatric HIV (prevalence, incidence, mortality, and ART coverage) for all Central Asian nations, particularly for specific age subgroups (e.g., 0-1 year, 1-5 years), are often limited or not publicly available.
Understanding HIV prevalence, incidence, and mortality in wider Central Asian countries is crucial, particularly given the region’s growing child population.11 Analyzing HIV dynamics in children under 5 in this region can inform targeted policies to support this vulnerable population.
The present study aimed to assess the prevalence, incidence, mortality, and health expenditures for HIV treatment in children under 5 years of age from 9 Central Asian countries (Armenia, Azerbaijan, Georgia, Kazakhstan, Kyrgyzstan, Mongolia, Tajikistan, Turkmenistan, Uzbekistan) and compare these findings with a global picture.
METHODS
Study design and population
This descriptive study includes prevalence, incidence and all deaths of children under 5 years of age attributed to HIV (ICD-11 codes B20-B24, C46-C469, D84.9; ICD-11 codes are 042-044, 112-118 (after 1980), 130 (after 1980), 136.3-136.8 (after 1980), 176.0-176.9 (after 1980), 279 (after 1980); and ICD-11 BTL codes are B184-B185), during the years 1990 to 2021 in 9 countries covered by Central Asia: Armenia, Azerbaijan, Georgia, Kazakhstan, Kyrgyzstan, Mongolia, Tajikistan, Turkmenistan, and Uzbekistan. Since most of the Central Asian countries in this study were part of the Soviet Union before 1991, we analyze trends.
Input data
The data collection protocol was described in detail in Figure S1.
Household seroprevalence surveys
Geographically representative HIV seroprevalence survey results were used as inputs to the model for countries with generalized HIV epidemics where available.
GBD demographic inputs
Location-specific population, fertility, migration, and HIV-free survival rates from GBD 2020 were used as inputs in modelling all locations.
Data from countries
The files compiled by the Joint United Nations Programme on HIV/AIDS (UNAIDS) for their HIV/AIDS estimation process were one of our sources of data for producing estimates of the HIV burden. The files are often built by within-country experts with the support of UNAIDS, which publishes estimates annually on behalf of countries and only shares their files when permission is granted. The files contain HIV-specific information needed to run the Spectrum1, Estimation and Projection Package-Age Sex2 (EPP-ASM) models. Spectrum and EPP-ASM require the following input data: AIDS mortality among people living with HIV with and without ART, CD4 progression among people living with HIV not on ART, ART coverage among adults and children, cotrimoxazole coverage among children, coverage of breastfeeding among women living with HIV, prevention of mother-to-child transmission coverage, and CD4 thresholds for treatment eligibility. EPP-ASM additionally uses HIV prevalence data from surveillance sites and representative surveys. Antenatal care (ANC), incidence, prevalence, and treatment coverage data from UNAIDS were used in modelling for all locations. We extracted all of this data from the proprietary format used by UNAIDS.
Vital and civil registration
We utilized all available sources of vital and civil registration, as well as sample registration data, from the GBD Causes of Death database, following the redistribution of garbage codes and the correction of HIV/AIDS mis-coding in Group 2A countries from the Central Asian region. Both systems are administered by the Centers for Disease Control and Prevention, of which the reported number of deaths due to HIV is archived.
Case notifications data
We searched for case notification data using the ECDC database and the country reports series in countries with four- and five-star vital registration data. We identified all nine countries for which information was available.
Prevalence Data
Geographically representative HIV seroprevalence survey results were used as inputs to the model for countries with generalized HIV epidemics where available. From these surveys, we used age- and sex specific prevalence data.
Data from countries
The files compiled by UNAIDS for their HIV/AIDS estimation process served as our primary source of data for producing estimates of the HIV burden. The files are often built by within-country experts with the support of UNAIDS, which publishes estimates annually on behalf of countries and only shares their files when permission is granted. The files contain HIV-specific information necessary to run the Spectrum4 Estimation and Projection Package-Age Sex (EPP-ASM)5 models. We extracted all of this data from the proprietary format used by UNAIDS. The EPP-ASM and Spectrum models used for GBD estimation vary slightly from those used by UNAIDS, with details on this variation included below. In addition to the differences in model structure, we integrate our estimates of input model parameters, including new transition parameters and demographic rates. The differences between our estimates and UNAIDS’ estimates reflect differences in model structure, model parameters, and the location-specific data used to calibrate our models.
Modelling strategy
The conceptual and analytical framework of the model was based on the Global Burden of Disease protocol (https://www.healthdata.org/sites/default/files/2024-06/GBD%20Protocol%20060424.pdf), a causal hierarchy, and detailed methods have been previously published by us.12-14 We used two different components to derive year-, age-, and sex-specific estimates of HIV incidence, prevalence, and mortality depending on the locations’ availability of data and extent of HIV burden, as described below:
- EPP-ASM was used to estimate incidence, prevalence, and mortality that are consistent with serosurveillance data from antenatal care clinics and/or prevalence surveys.
- Spectrum is a compartmental HIV progression model used to generate age-sex-specific incidence, prevalence, and death rates from input incidence and prevalence curves and assumptions about intervention scale-up and local variation in epidemiology. This model was used in conjunction with EPP-ASM for India and for all Group 2A countries.
Statistical analysis
The data were analyzed using SPSS version 21 software. The data were reported as numbers, percentages, mean, and standard deviation. The data were separated by gender and place of residence. The mortality rate was calculated per 10,000 live births. To visually represent the mortality rate of children under 5 years of age attributed to HIV, we used ArcGIS software (version 1.10). These maps highlight areas within the studied regions and countries. Distinct colors were employed to differentiate areas based on their varying mortality rates.
RESULTS
Global and national scenario (Overall estimates)
The global HIV burden has grown significantly over the past three decades. HIV-related deaths rose nearly threefold, from 305,944 in 1990 to 863,837 in 2019, while prevalence increased from 7.93 million to 36.85 million cases during the same period. In Central Asia, the epidemic escalated sharply. HIV-related deaths rose from 401 in 1990 to 27,715 in 2019—a 69-fold increase. Prevalence also surged from 4,776 to 1.54 million cases. Kazakhstan and Uzbekistan were the most affected. In Kazakhstan, deaths increased from 96 to 261; Uzbekistan recorded the highest rise in deaths, from 120 to 585 (a 385% increase), and in new cases, from 804 to 2,537 (Table 1). In contrast, Georgia showed a decline in new HIV cases, dropping from 477 in 1990 to 269 in 2019. Kyrgyzstan and Tajikistan experienced moderate increases in deaths—Kyrgyzstan’s rose more than fourfold, and Tajikistan’s by 41%. Mongolia remained the least affected, with a minimal rise in deaths (from 8 to 15) and new cases (from 35 to 39) over the same period.
| Table 1. Number of deaths due to HIV, number of new HIV acquired cases, number of prevalent cases due to HIV between 1990 and 2019 for GBD super-regions and nine countries in the Central Asian region | ||||||
| GBD super-regions |
|
|
|
|||
|
|
|
|
|
|
|
|
| Global |
404,774.04) |
|
2,181,339.29 7) |
|
8,495,409.73) |
38,856,666.01) |
| Central Asia |
|
|
|
|
|
|
| Armenia |
|
|
|
|
|
|
| Azerbaijan |
|
|
|
|
|
|
| Georgia |
|
|
|
|
|
|
| Kazakhstan |
|
|
|
|
|
|
| Kyrgyzstan |
|
|
|
|
|
|
| Mongolia |
|
|
|
|
|
|
| Tajikistan |
|
|
|
|
|
|
| Turkmenistan |
|
|
|
|
|
|
| Uzbekistan |
|
|
|
|
|
|
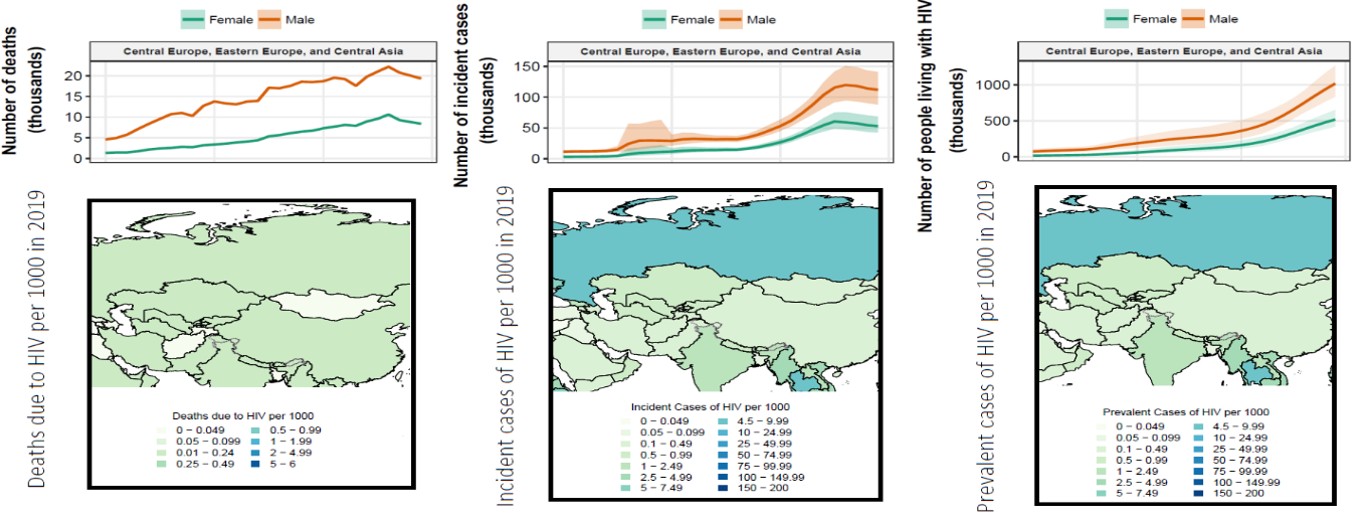
Sex difference
Across all three metrics, males consistently demonstrate higher numerical values than females. The line graphs suggest that over time, the number of deaths attributable to HIV has been increasing for both sexes, but the escalation is more pronounced in males. Correspondingly, the number of newly acquired HIV cases has been growing, with men experiencing a more precipitous rise compared to women. The prevalence of HIV, denoting the total population living with the virus, also follows this pattern, with a steeper upward trend in males than in females (Figure 1).
Under 5 years of age children scenario
The scenario for children under 5 years of age is presented in Table 2. The data on HIV-related deaths, incidence cases, and prevalent cases from 1990 to 2019 reveal significant trends in the global and Central Asian contexts. In 1990, the number of deaths due to HIV globally was 43,744.40 (95% CI: 38,062.46 - 48,832.55), but by 2019, this figure significantly decreased to 20,594.30 (95% CI: 15,723.78 - 27,328.31), reflecting a significant reduction in mortality. In Central Asia, however, the number of deaths remained relatively stable, increasing slightly from 24.70 (95% CI: 24.69 - 24.71) in 1990 to 25.80 (95% CI: 25.75 - 25.85) in 2019, indicating persistent challenges in this region. Among individual Central Asian countries, Kazakhstan, Kyrgyzstan, and Uzbekistan exhibited variations in mortality trends (Figure S2). Kazakhstan’s HIV-related deaths increased slightly from 2.15 (95% CI: 2.14 - 2.15) in 1990 to 2.42 (95% CI: 2.41 - 2.42) in 2019. In Kyrgyzstan, the death toll also rose from 1.73 (95% CI: 1.73 - 1.74) in 1990 to 2.25 (95% CI: 2.25 - 2.26) in 2019. Meanwhile, Uzbekistan experienced a more noticeable increase, from 10.06 (95% CI: 10.05-10.07) in 1990 to 11.52 (95% CI: 11.49-11.55) in 2019.
| Table 2. Number of deaths due to HIV, number of new HIV acquired cases, number of prevalent cases due to HIV between 1990 and 2019 for GBD super-regions and nine countries in the Central Asian region in children under 5 years of age | ||||||
| GBD super-regions |
|
|
|
|||
|
|
|
|
|
|
|
|
| Global |
|
|
|
|
|
|
| Central Asia |
|
|
|
|
|
|
| Armenia |
|
|
|
|
|
|
| Azerbaijan |
|
|
|
|
|
|
| Georgia |
|
|
|
|
|
|
| Kazakhstan |
|
|
|
|
|
|
| Kyrgyzstan |
|
|
|
|
|
|
| Mongolia |
|
|
|
|
|
|
| Tajikistan |
|
|
|
|
|
|
| Turkmenistan |
|
|
|
|
|
|
| Uzbekistan |
|
|
|
|
|
|
The global number of new HIV-acquired cases decreased substantially, from 256,869.86 (95% CI: 232,181.80-280,576.59) in 1990 to 101,273.76 (95% CI: 84,106.23-126,532.44) in 2019. In contrast, Central Asia saw an increase in incidence cases from 82.55 (95% CI: 53.41 - 123.31) in 1990 to 128.36 (95% CI: 77.12 - 280.88) in 2019, suggesting ongoing transmission despite global progress. Notably, Kazakhstan’s incidence cases surged from 26.27 (95% CI: 16.03 - 39.22) in 1990 to 41.59 (95% CI: 26.38 - 67.70) in 2019, while Kyrgyzstan experienced an alarming rise from 2.63 (95% CI: 1.48 - 4.61) in 1990 to 33.21 (95% CI: 11.77 - 141.28) in 2019 (Figure S3).
HIV prevalence, reflecting the total number of living cases, slightly increased globally from 290,331.34 (95% CI: 265,698.46 - 316,063.71) in 1990 to 294,367.71 (95% CI: 251,093.66 - 357,920.66) in 2019. In Central Asia, however, prevalence nearly doubled from 55.83 (95% CI: 38.25 - 77.53) in 1990 to 103.88 (95% CI: 53.13 - 267.47) in 2019, indicating persistent transmission and an increasing number of people living with HIV. Countries such as Kazakhstan and Kyrgyzstan showed a sharp rise in prevalence, with Kazakhstan increasing from 7.35 (95% CI: 4.87 - 10.40) in 1990 to 24.51 (95% CI: 12.18 - 70.48) in 2019, and Kyrgyzstan from 2.51 (95% CI: 1.47 - 4.01) in 1990 to 20.19 (95% CI: 5.93 - 74.93) in 2019 (Figure S4).
Figure 2 illustrates the HIV-related deaths, incidence cases, and prevalent cases among children under 5 years old per 1,000 individuals globally. In 1990, the highest prevalence of HIV in children under five was concentrated in Sub-Saharan Africa, with some countries experiencing over 500 cases per 100,000. By 2021, the prevalence had significantly declined globally, yet Sub-Saharan Africa remained the most heavily impacted region. The incidence of new HIV acquired cases in 1990 followed a similar pattern, with the highest rates in Sub-Saharan Africa, as well as some cases in parts of South America and Southeast Asia. By 2021, there was a substantial decrease in new cases globally, with improvements in regions that had previously experienced high burdens. Mortality rates due to HIV in children under five were also highest in Sub-Saharan Africa in 1990. However, by 2021, there was a notable reduction in child deaths from HIV, reflecting advancements in treatment, prevention, and intervention programs. Whereas in Central Asian countries, there was a surge in HIV incidence in children under 5 years of age.
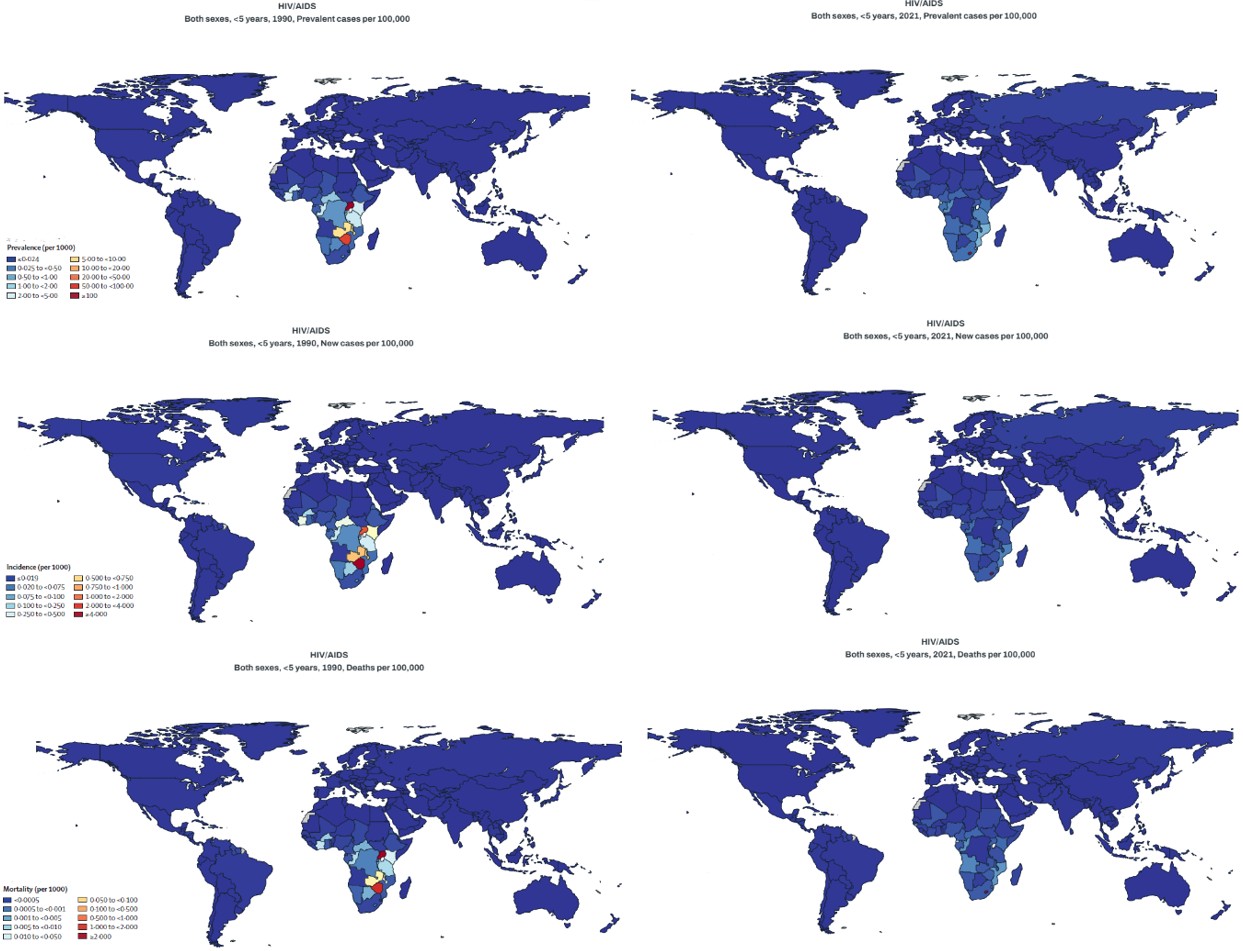
Overall, the comparison of these maps indicates that while the global burden of HIV in children under five has declined significantly from 1990 to 2021, Sub-Saharan Africa remains the most affected region. The improvements seen over time are likely due to the expansion of HIV treatment, prevention of mother-to-child transmission, and public health initiatives aimed at reducing HIV-related mortality among young children.
Sex difference in the under-5-year age group
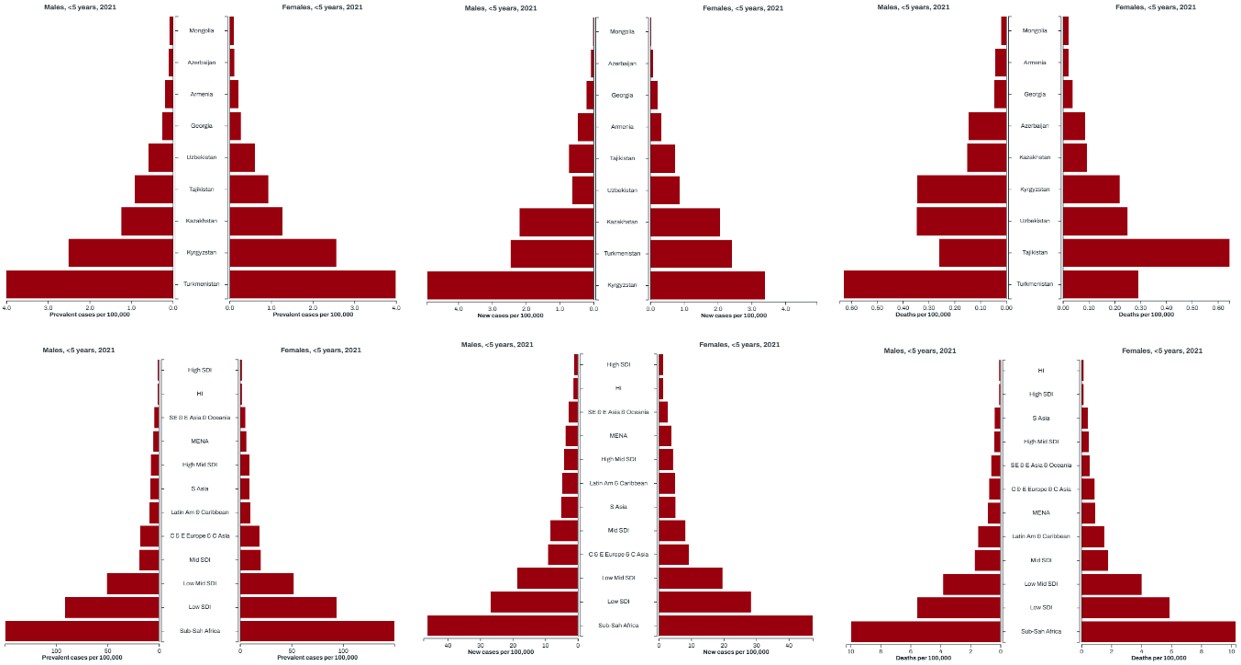
The data presented in Figure 3 highlight notable sex-based disparities in HIV-related mortality, incidence, and prevalence among children under 5 years of age across global and regional levels, particularly in Central Asia. Overall, HIV-related deaths among young boys have consistently been higher than in girls, both globally and in Central Asia. In terms of prevalence in 2021, the highest burden is observed in Kyrgyzstan, Tajikistan, and Uzbekistan for both males and females. These countries exhibit significantly higher prevalence rates compared to other nations in the dataset. The broader regional estimates indicate that Sub-Saharan Africa has the highest prevalence, followed by lower-middle-income countries, while high-income countries have the lowest rates. The incidence of new cases of HIV per 100,000 in 2021 displays a similar pattern. Countries such as Kyrgyzstan, Tajikistan, and Uzbekistan report the highest rates for both males and females. In the regional estimates, Sub-Saharan Africa again records the highest incidence rates, with lower-middle-income countries following closely behind. Regarding mortality, the death rates per 100,000 in 2021 suggest that Kyrgyzstan and Tajikistan have the highest mortality burden among the selected countries.
HIV total health spending
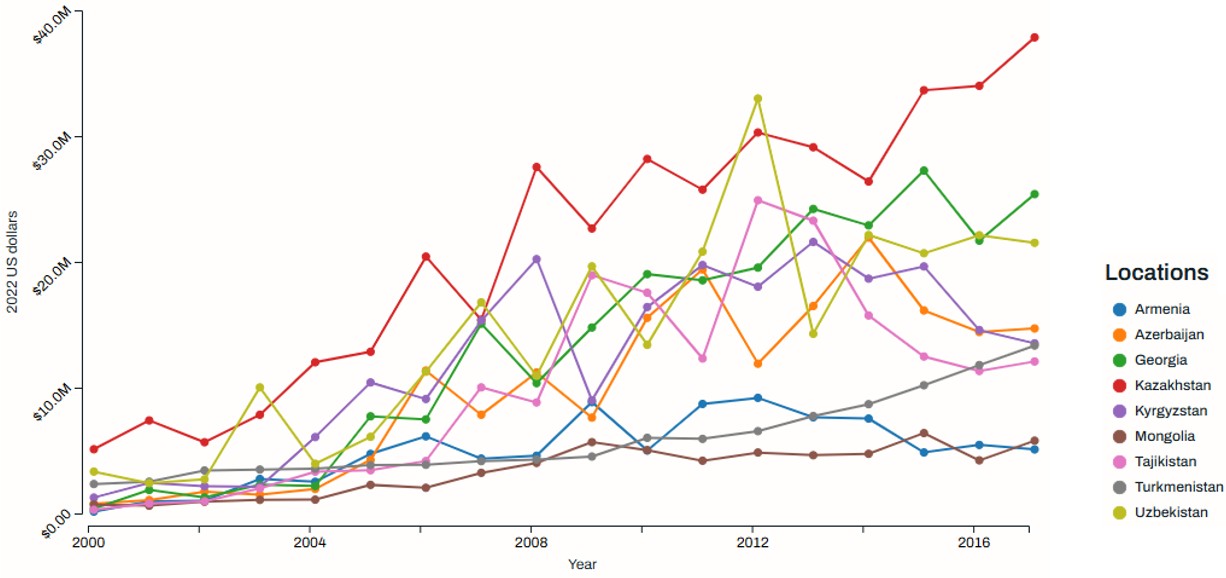
Figure 4 illustrates the trends in HIV total health spending in Central Asian countries from 2000 to 2017, expressed in 2022 US dollars. The data indicate that HIV healthcare expenditures have risen across the board, demonstrating a heightened commitment to combating the epidemic. Nevertheless, spending levels have experienced notable variations for certain countries. Kazakhstan consistently had the highest spending among the countries shown. The spending saw steady growth, with sharp increases around 2004–2006 and another significant rise after 2012. By 2017, Kazakhstan’s spending had exceeded $40 million, making it the dominant country in terms of financial commitment to HIV/AIDS healthcare. Mid-tier spending countries such as Georgia, Kyrgyzstan, and Uzbekistan have relatively higher spending than others, although their trends are more volatile. Georgia experienced notable peaks around 2012 and 2016, while Kyrgyzstan maintained a moderate level of spending despite some fluctuations. In contrast, lower spending countries, including Armenia, Azerbaijan, Mongolia, Tajikistan, and Turkmenistan, have consistently allocated less to HIV healthcare. Their spending remained below $10 million for most of the period. Among them, Turkmenistan and Mongolia have the lowest and most stable spending trends, with only slight increases over time.
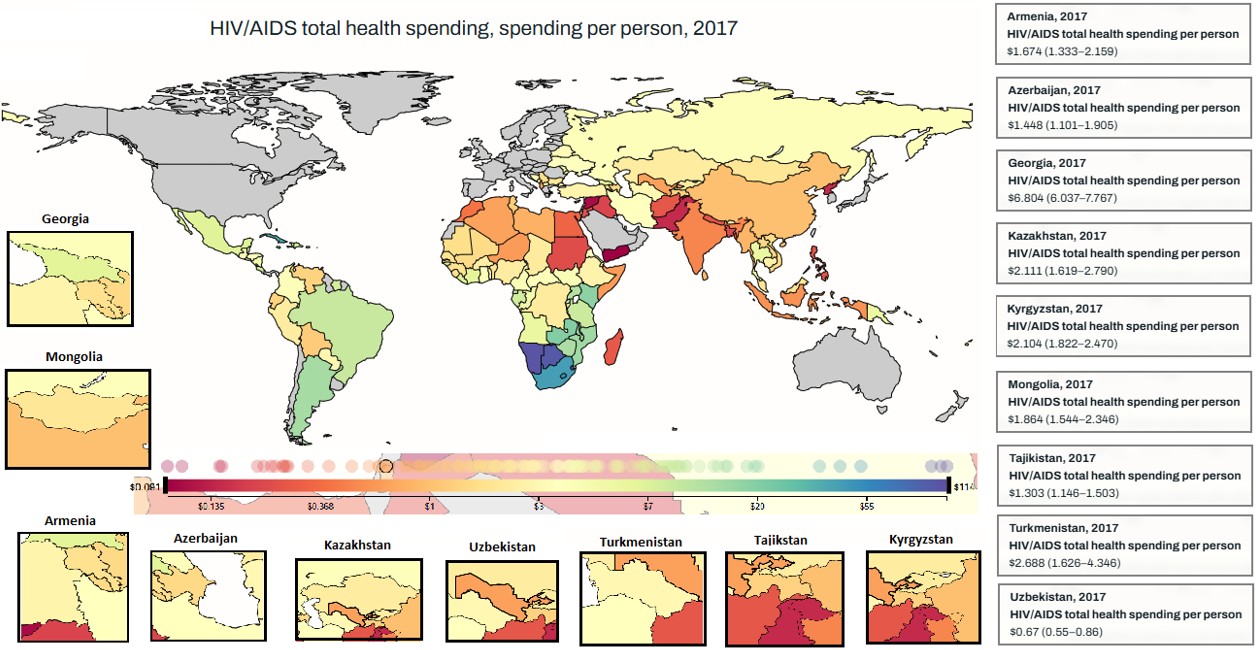
Figure 5 presents the total health spending per person in Central Asian countries for the year 2017. It shows significant variation in spending levels, with some countries allocating considerably more resources per capita than others. Kazakhstan had the highest per-person spending on HIV, reaching $2.11. Kyrgyzstan followed with a spending of $2.10 per person, which is relatively close to Kazakhstan’s level. Tajikistan’s per-person spending on HIV healthcare was slightly lower at $1.30, while Mongolia and Armenia allocated moderate resources, with per capita expenditures of $1.84 and $1.67, respectively. At the lower end of the spectrum, Azerbaijan and Turkmenistan had even lower spending levels, with Azerbaijan at $1.48 per person and Turkmenistan at $0.82 per person. Notably, Uzbekistan had the lowest per capita spending on HIV among all the Central Asian countries represented, at just $0.70.
DISCUSSION
The findings of this study highlight the alarming increase in HIV-related prevalence, incidence, and mortality among children under five years of age in Central Asian countries. The global burden of HIV-related deaths and cases has seen a significant decline due to advancements in antiretroviral therapy, prevention strategies, and improved healthcare access.15 Recent studies indicate gaps in data on HIV under-5 prevalence, incidence, and mortality in the Central Asian region.16 Our study revealed that in Central Asia, the situation remains a significant concern as mortality rates, prevalence, and new cases continue to rise, indicating gaps in prevention and treatment programs.
Central Asia faces one of the highest rates of IDU globally, mainly due to heroin trafficking from Afghanistan.17,18 Efforts to curb transmission were further hindered by restrictive policies—Uzbekistan, for instance, banned methadone until 2019, delaying effective opioid substitution therapy (OST) and exacerbating HIV outbreaks among PWID.19 According to UNAIDS (2023), only 50% of people living with HIV in Eastern Europe and Central Asia were receiving antiretroviral therapy (ART), far below global targets.20 Additionally, labor migration and unprotected sex work contributed to secondary transmission, with condom use among key populations remaining critically low.21,22
In contrast to Central Asia’s escalating HIV crisis, Georgia achieved a significant decline in new HIV cases through a robust and systematic public health response.23,24 A critical turning point came in 2018, when Georgia decriminalized drug use, removing legal barriers and encouraging higher uptake of HIV testing and treatment.24
In children under five years old, the data reveal a stark contrast between global and regional trends. While global HIV-related mortality in this age group has declined significantly, Central Asia experienced a slight increase.25 There are several reasons affecting this, such as delayed Diagnosis and Treatment Initiation, barriers to access to care, and stigma. Low rates of HIV testing in children, often due to fear of discrimination and stigma, result in late diagnoses.26,27 Without early detection and prompt initiation of ART, HIV rapidly progresses in young children, leading to severe opportunistic infections and higher mortality rates. In the Eastern European and Central Asian (EECA) region, which includes Central Asia, only a fraction of children living with HIV are on treatment, lagging significantly behind adult coverage. Moreover, 50% of the ART access rate affects prevention, and the new case emergency rate is at 20%. This trend underscores the need for stronger regional healthcare policies, enhanced maternal screening programs, and improved perinatal care to mitigate mother-to-child transmission of HIV.
Gender disparities in HIV-related prevalence, incidence, and mortality were also evident in the study. Across Central Asia, males exhibited higher mortality and prevalence rates than females. This is different from the global trend; following UNAIDS, women account for 49% of HIV worldwide.28
The data indicate substantial global advancements in mitigating HIV-associated mortality and new infections. However, Central Asia, particularly Kazakhstan and Kyrgyzstan, represents a concerning region due to the escalating incidence and prevalence of cases. These findings underscore the need for targeted interventions, improved healthcare accessibility, and strengthened prevention strategies in this region. Another key finding was the significant variation in health expenditures dedicated to HIV across Central Asian countries. Kazakhstan emerged as the highest spender on HIV healthcare, with over $40 million allocated in 2017, whereas Uzbekistan had the lowest per capita expenditure, at just $0.70 per person. UNAIDS indicated $34/person target for HIV prevention, which is not met by any of the Central Asian countries.29 80% of Central Asian countries’ health expenditures rely on international donors; however, this is changing due to the shift of some countries to the middle-income group, contributing to unstable HIV financing. These disparities highlight the varying levels of commitment and resource allocation for HIV prevention and treatment across the region, emphasizing the need for equitable healthcare investments.
Today, in developed and industrialized countries, with timely diagnosis and treatment of HIV-infected infants and children29, clinical manifestations of HIV in children are rare. Almost all of them reach adolescence, youth, and adulthood without clinical symptoms due to immunodeficiency. Their main problems are the continued use of antiviral drugs, drug resistance, drug side effects, psychological distress, social problems, and sexual and marital issues.30 However, in developing countries where HIV in pregnant mothers and their infants is not diagnosed (due to lack of screening), perinatal acquisition of HIV (without antiretroviral treatment) shows one of the following three clinical scenarios.31,32
The first scenario, untreated HIV-positive cases have a rapidly progressive course, become symptomatic in the first months of life, and have a median half-life of 6-9 months. These infants are most likely to have been infected in utero and have a positive HIV-related Polymerase chain reaction (PCR) within the first 48 hours of birth. Almost all children with a rapidly progressive course die before the age of 5 years.33 The second scenario, which is predominantly HIV-positive (untreated) infants, has a gradually progressive course and becomes symptomatic in the first or second year of life. These children appear to have acquired HIV perinatally or postnatally through breastfeeding. Most of these children are PCR-positive in the first month of life and survive to the age of 5 years.34 The third scenario includes patients with perinatal HIV whose disease (without treatment) has a very slow course and is clinically asymptomatic until after the age of 10 years, and has an increased CD4 count.35,36
Until recently, it was thought that few children with perinatally acquired (untreated) HIV survived the age of 5 years, but recent studies have shown that less than 18% of these children survive to the age of 15 years without treatment.37 Children infected after birth and through breastfeeding appear to have a greater predisposition to a slow course of HIV than those who acquire the virus in utero or at birth.38 Contrary to expectations, the percentage of HIV-positive children with a slow course is higher in Africa than in developed countries, where 1.3% of children with perinatal acquired HIV have a slow course and, without treatment, their average life expectancy is 16 years.39 This difference seems to be because in developed countries, HIV transmission through breast milk is virtually non-existent, and all HIV-positive children are infected during delivery or before birth. In contrast, in less developed countries, up to half of HIV-positive children are infected through breast milk.40 In a cohort study from Latin America on HIV acquired adolescents, approximately one-third of them were first diagnosed with HIV after the age of 10.41,42
Child mortality (under 5 years) is a phenomenon influenced by several factors and conditions, and the severity and weakness of these factors and conditions determine the occurrence and prevalence of mortality, as well as its control. Another important point that should be mentioned is that infant and child mortality is affected by a set of socioeconomic, cultural, demographic, genetic, and medical-health variables.43,44
Study limitations
Despite the comprehensive nature of this study, several limitations must be acknowledged. Firstly, the study relies on mortality registration systems, which may have data inconsistencies, underreporting, or misclassification of deaths related to HIV. Stigma-driven underreporting could contribute to a 30-50% reduction in statistics. For instance, the United Nations International Children’s Emergency Fund (UNICEF) reported that approximately 50% of HIV-exposed infants in Uzbekistan receive PCR testing.45 Secondly, the availability and accuracy of data for Central Asian countries vary, which may impact the reliability of country-specific estimates. Data consistency varies according to country settings. For instance, Kazakhstan and Kyrgyzstan publish annual HIV surveillance reports, mother-to-child transmission rates, and ART coverage data. In contrast, Tajikistan and Uzbekistan publish aggregated data, while Turkmenistan’s data rely on WHO and UNAIDS estimates. Thirdly, the study does not account for the impact of more recent antiretroviral treatment programs or emerging healthcare policies that could influence HIV trends beyond 2019. Lastly, socioeconomic and cultural factors affecting HIV transmission and healthcare access were not deeply explored, warranting further qualitative studies.
Implications for clinical practice
The study findings have critical implications for clinical practice and public health policy. To reduce pediatric HIV-related mortality in Central Asia, a multifaceted approach is needed. Universal maternal screening and programs to prevent mother-to-child transmission (PMTCT) should be prioritized. Routine prenatal HIV testing must be integrated into maternal healthcare, following successful models from high-income countries. Ensuring that all HIV-positive pregnant women receive antiretroviral therapy (ART) is essential to minimizing perinatal transmission.
Expanding ART access and strengthening neonatal care services are critical components in improving pediatric HIV outcomes. Early ART initiation for HIV-exposed infants can significantly reduce mortality, while enhancing neonatal intensive care units (NICUs) can provide specialized support for HIV-infected newborns. Improving ART supply chains, training healthcare professionals, and addressing barriers to timely treatment initiation will also contribute to better health outcomes.
Addressing healthcare disparities across Central Asian countries is necessary to bridge the gap between high- and low-investment nations. Increased healthcare funding, particularly in low-resource settings, can ensure equitable access to prevention and treatment services. Community-based HIV programs should be expanded, especially in rural and underserved regions, to enhance early detection and adherence to treatment.
Gender-sensitive interventions should be incorporated into HIV prevention and treatment strategies. Further research is needed to understand the underlying factors contributing to higher HIV-related mortality and prevalence among males. Developing targeted interventions that consider gender-specific vulnerabilities will help improve overall health outcomes for children under five.
Policy and funding reforms must be prioritized to strengthen national responses to pediatric acquired HIV. Governments should increase financial commitments to HIV programs and seek international aid to support prevention and treatment efforts. Strengthening collaboration with global health organizations and implementing evidence-based policies will help reduce pediatric HIV-related mortality in Central Asia and improve healthcare accessibility for affected children.
CONCLUSION
This study highlights the escalating HIV burden in Central Asia, particularly among children under five years old. While global trends show a decline in HIV-related mortality and incidence, Central Asian countries continue to struggle with rising cases and limited healthcare resources. Increasing investments in maternal screening, antiretroviral therapy, and neonatal healthcare facilities are essential to curb pediatric HIV-related mortality. Increasing the equipment and facilities of neonatal intensive care units can play an effective role in reducing child mortality. Future policies should prioritize equitable healthcare access, improve data accuracy, and address gender disparities in HIV outcomes. By implementing comprehensive prevention and treatment strategies, the region can make significant progress in reducing HIV-related mortality and improving the quality of life for affected children. Comprehensive strategies for the prevention of mother-to-child transmission (PMTCT) of HIV, diagnosis of HIV in pregnant women and perinatal acquired HIV, initiation of timely and appropriate antiretroviral therapy, as well as prevention of opportunistic infection, can help the region make significant progress in reducing HIV-related mortality and improving the quality of life of affected children.
Ethical approval
This study has been approved by the Osh State University (number OSHSU-021-5564). Written informed consent was obtained from the participants.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Fauci AS, Lane HC. Human immunodeficiency virus disease: AIDS and related disorders. In: Jameson JL, Fauci AS, Kasper DL, et al. editors. Harrison’s principles of internal medicine. 20th ed. New York: McGraw-Hill; 2018.
- Lule F. Global burden of HIV/AIDS. In: Haring R, Kickbusch I, Ganten D, Moeti M, editors. Handbook of global health. Cham: Springer International Publishing; 2020: 1-49. https://doi.org/10.1007/978-3-030-05325-3_31-1
- DeGruttola V, Little S, Schooley R. Controlling the HIV epidemic, without a vaccine!. AIDS. 2008;22:2554-5. https://doi.org/10.1097/QAD.0b013e32831940d3
- Moyo E, Moyo P, Murewanhema G, Mhango M, Chitungo I, Dzinamarira T. Key populations and Sub-Saharan Africa’s HIV response. Front Public Health. 2023;11:1079990. https://doi.org/10.3389/fpubh.2023.1079990
- Gaparalievich KK, Rahim F, Kalmatov R, Dzhusupov K, Mitalipovna BM. HIV in children under 5 years of age, and its health expenditure in Central Asian countries. Indian J Pediatr. 2025;92:560. https://doi.org/10.1007/s12098-025-05484-z
- UNICEF. 2023 HIV and AIDS in Eastern Europe and Central Asia Snapshot. 2023. Available at: https://www.unicef.org/eca/documents/2023-hiv-and-aids-eastern-europe-and-central-asia-snapshot
- World Health Organization (WHO) Europe. HIV/AIDS Surveillance in Europe and Central Asia 2022. Copenhagen: WHO Regional Office for Europe; 2023. Available at: https://www.who.int/europe/publications/i/item/9789289058543
- Paintsil E, Andiman WA. Update on successes and challenges regarding mother-to-child transmission of HIV. Curr Opin Pediatr. 2009;21:94-101. https://doi.org/10.1097/MOP.0b013e32831ec353
- Cerveny L, Murthi P, Staud F. HIV in pregnancy: mother-to-child transmission, pharmacotherapy, and toxicity. Biochim Biophys Acta Mol Basis Dis. 2021;1867:166206. https://doi.org/10.1016/j.bbadis.2021.166206
- Njom Nlend AE. Mother-to-child transmission of HIV through breastfeeding improving awareness and education: a short narrative review. Int J Womens Health. 2022;14:697-703. https://doi.org/10.2147/IJWH.S330715
- World Bank. Fertility rate, total (births per woman) - Central Asia. 2024. Available at: https://data.worldbank.org/indicator/SP.DYN.TFRT.IN (Accessed on July 10, 2024).
- GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736-88. https://doi.org/10.1016/S0140-6736(18)32203-7
- GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1859-922. https://doi.org/10.1016/S0140-6736(18)32335-3
- GBD 2017 HIV collaborators. Global, regional, and national incidence, prevalence, and mortality of HIV, 1980-2017, and forecasts to 2030, for 195 countries and territories: a systematic analysis for the Global Burden of Diseases, Injuries, and Risk Factors Study 2017. Lancet HIV. 2019;6:e831-59. https://doi.org/10.1016/S2352-3018(19)30196-1
- Rodríguez-Zúñiga MJM, Heath MS, Gontijo JRV, Ortega-Loayza AG. Pyoderma gangrenosum: a review with special emphasis on Latin America literature. An Bras Dermatol. 2019;94:729-43. https://doi.org/10.1016/j.abd.2019.06.001
- UNAIDS. The path that ends AIDS: UNAIDS Global AIDS Update 2023. Geneva: Joint United Nations Programme on HIV/AIDS (UNAIDS); 2023. Available at: https://www.unaids.org/en/resources/documents/2023/global-aids-update-2023
- Mathers BM, Degenhardt L, Phillips B, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet. 2008;372:1733-45. https://doi.org/10.1016/S0140-6736(08)61311-2
- Thorne C, Ferencic N, Malyuta R, Mimica J, Niemiec T. Central Asia: hotspot in the worldwide HIV epidemic. Lancet Infect Dis. 2010;10:479-88. https://doi.org/10.1016/S1473-3099(10)70118-3
- Des Jarlais DC, Arasteh K, Semaan S, Wood E. HIV among injecting drug users: current epidemiology, biologic markers, respondent-driven sampling, and supervised-injection facilities. Curr Opin HIV AIDS. 2009;4:308-13. https://doi.org/10.1097/COH.0b013e32832bbc6f
- UNAIDS. Eastern Europe and Central Asia regional profile. UNAIDS; 2024. Available at: https://www.unaids.org/sites/default/files/media_asset/2024-unaids-global-aids-update-eeca_en.pdf (Accessed on June 15, 2025).
- Liu SH, Srikrishnan AK, Zelaya CE, Solomon S, Celentano DD, Sherman SG. Measuring perceived stigma in female sex workers in Chennai, India. AIDS Care. 2011;23:619-27. https://doi.org/10.1080/09540121.2010.525606
- Steen R, Hontelez JAC, Mugurungi O, et al. Economy, migrant labour and sex work: interplay of HIV epidemic drivers in Zimbabwe over three decades. AIDS. 2019;33:123-31. https://doi.org/10.1097/QAD.0000000000002066
- Otiashvili D, Kirtadze I, Vardanashvili I, Tabatadze M, Ober AJ. Perceived acceptability of and willingness to use syringe vending machines: results of a cross-sectional survey of out-of-service people who inject drugs in Tbilisi, Georgia. Harm Reduct J. 2019;16:21. https://doi.org/10.1186/s12954-019-0292-8
- DeBeck K, Cheng T, Montaner JS, et al. HIV and the criminalisation of drug use among people who inject drugs: a systematic review. Lancet HIV. 2017;4:e357-74. https://doi.org/10.1016/S2352-3018(17)30073-5
- Purcell DJ, Standifer M, Martin E, Rivera M, Hopkins J. Disparities in HIV care: a rural-urban analysis of healthcare access and treatment adherence in Georgia. Healthcare (Basel). 2025;13:1374. https://doi.org/10.3390/healthcare13121374
- World Health Organization (WHO). Treatment and care in children and adolescents. Global HIV Programme. Available at: https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/hiv/treatment/treatment-and-care-in-children-and-adolescents (Accessed on June 15, 2025).
- UNICEF. HIV - Paediatric care and treatment. UNICEF DATA. Available at: https://data.unicef.org/topic/hivaids/paediatric-treatment-and-care/ (Accessed on June 15, 2025).
- The Lancet Hiv. Addressing inequalities still key to ending HIV/AIDS. Lancet HIV. 2023;10:e1. https://doi.org/10.1016/S2352-3018(22)00376-9
- Judd A, Collins IJ, Parrott F, et al. Growing up with perinatal HIV: changes in clinical outcomes before and after transfer to adult care in the UK. J Int AIDS Soc. 2017;20:21577. https://doi.org/10.7448/IAS.20.4.21577
- Nguyen DT, Graviss EA. Diabetic trends and associated mortality in tuberculosis patients in Texas, a large population-based analysis. Tuberculosis (Edinb). 2019;116S:S59-65. https://doi.org/10.1016/j.tube.2019.04.011
- Sayyah M, Rahim F, Kayedani GA, Shirbandi K, Saki-Malehi A. Global view of HIV prevalence in prisons: a systematic review and meta-analysis. Iran J Public Health. 2019;48:217-26.
- Grant AD, De Cock KM. The growing challenge of HIV/AIDS in developing countries. Br Med Bull. 1998;54:369-81. https://doi.org/10.1093/oxfordjournals.bmb.a011694
- Sandbulte MR, Gautney BJ, Maloba M, et al. Infant HIV testing at birth using point-of-care and conventional HIV DNA PCR: an implementation feasibility pilot study in Kenya. Pilot Feasibility Stud. 2019;5:18. https://doi.org/10.1186/s40814-019-0402-0
- Tobin NH, Aldrovandi GM. Immunology of pediatric HIV infection. Immunol Rev. 2013;254:143-69. https://doi.org/10.1111/imr.12074
- Merchant RH, Lala MM. Common clinical problems in children living with HIV/AIDS: systemic approach. Indian J Pediatr. 2012;79:1506-13. https://doi.org/10.1007/s12098-012-0865-y
- Ofori-Mante JA, Kaul A, Rigaud M, et al. Natural history of HIV infected pediatric long-term or slow progressor population after the first decade of life. Pediatr Infect Dis J. 2007;26:217-20. https://doi.org/10.1097/01.inf.0000254413.11246.e1
- Mutanga JN, Mutembo S, Ezeamama AE, et al. Long-term survival outcomes of HIV infected children receiving antiretroviral therapy: an observational study from Zambia (2003-2015). BMC Public Health. 2019;19:115. https://doi.org/10.1186/s12889-019-6444-7
- Ellington SR, King CC, Kourtis AP. Host factors that influence mother-to-child transmission of HIV-1: genetics, coinfections, behavior and nutrition. Future Virol. 2011;6:1451-69. https://doi.org/10.2217/fvl.11.119
- Ferrand RA, Corbett EL, Wood R, et al. AIDS among older children and adolescents in Southern Africa: projecting the time course and magnitude of the epidemic. AIDS. 2009;23:2039-46. https://doi.org/10.1097/QAD.0b013e32833016ce
- Kuhn L, Aldrovandi G. Survival and health benefits of breastfeeding versus artificial feeding in infants of HIV-infected women: developing versus developed world. Clin Perinatol. 2010;37:843-62, x. https://doi.org/10.1016/j.clp.2010.08.011
- Santos Cruz ML, Freimanis Hance L, Korelitz J, et al. Characteristics of HIV infected adolescents in Latin America: results from the NISDI pediatric study. J Trop Pediatr. 2011;57:165-72. https://doi.org/10.1093/tropej/fmq068
- Okobi OE, Ibanga IU, Egbujo UC, Egbuchua TO, Oranu KP, Oranika US. Trends and factors associated with mortality rates of leading causes of infant death: a CDC Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) database analysis. Cureus. 2023;15:e45652. https://doi.org/10.7759/cureus.45652
- Khadka KB, Lieberman LS, Giedraitis V, Bhatta L, Pandey G. The socio-economic determinants of infant mortality in Nepal: analysis of Nepal Demographic Health Survey, 2011. BMC Pediatr. 2015;15:152. https://doi.org/10.1186/s12887-015-0468-7
- Kammerlander A, Schulze GG. Local economic growth and infant mortality. J Health Econ. 2023;87:102699. https://doi.org/10.1016/j.jhealeco.2022.102699
- UNICEF. Children and HIV in Central Asia: a statistical snapshot. 2022. Available at: https://data.unicef.org
Copyright and license
Copyright © 2025 The author(s). This is an open-access article published by Aydın Pediatric Society under the terms of the Creative Commons Attribution License (CC BY) which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.